Healthy Starts for Healthier Lives: Research Impacts 2012 – 2019
Table of Contents
- Scientific Director's Message
- Strategic Approach
- IHDCYH in Numbers
- Healthy Developmental Trajectories
- Healthy Reproduction, Pregnancy, Childhood and Youth
- Healthy Public Policy and Systems Integration
- Enabling Tactics
- Thanks
- Appendix 1: Funding committed from 2012 to 2019
Scientific Director’s Message
It is with great pride but also some sadness that I write this message. It has been a privilege and honour to steer the CIHR Institute of Human Development, Child and Youth Health (IHDCYH) for almost a decade as the Scientific Director, and as a champion for our community of researchers, policy makers, patient partners, children, youth and families.
This report highlights innovative and impactful research funded while I was Scientific Director. By developing and funding broad reaching initiatives, as well as more focused activities in concert with our many partners and stakeholders, IHDCYH has been the catalyst for improvements to the health of children and families. However, the most praise for those improvements should go to all those who are involved in and carry out the work we fund.
IHDCYH’s strategic priorities during my tenure were developed in consultation with our community. In addressing these priorities, it was important to me to support our community to not only achieve research excellence, but also to embrace new models of funding to support innovative research approaches, to grow and support a pipeline for research capacity, and to inform and incorporate important advances in research policy in maternal, reproductive, child and youth health research in Canada. Ways in which we achieved this include:
- Moved from a disease-based to a life-trajectory approach to health research through the Healthy Life Trajectories Initiative (HeLTI)
- Brought together the perinatal, newborn and child development communities to approach preterm birth research as a continuous spectrum from conception to childhood through the Preterm Birth Network
- Created a collaborative team-based environment that enables the integration of clinical experience and insight into research in obstetrics and maternal-fetal medicine through the Clinician-Investigator Teams
- Brought together metadata from pregnancy and birth cohorts all over Canada to drive collaborative, high-powered big data research forward through the Research Advancement through Cohort Cataloguing and Harmonization (ReACH) initiative
Of course, this message also marks the end of my tenure at CIHR and more free time to go fishing! With the appointment of Dr. Christine Chambers as the next IHDCYH SD, the Institute is in good hands. I would like to sincerely thank everyone who has played a role in IHDCYH’s work including the CIHR leadership and Science Council members, our past and present Institute Advisory Board members, the IHDCYH and CIHR staff, and everyone who has contributed to this report.
Strategic Approach
IHDCYH’s Mission: Support research that ensures the best start in life for all Canadians and the achievement of their potential for optimal growth and development.
In 2012, a broad community consultation was used to generate IHDCYH’s Strategic Plan 2013–2017: Healthy Foundations of Life, which was updated in our 2018-20 Refreshed Strategic Plan. Our community directed us to target three overarching research investment themes with six specific strategic priorities. The five enabling tactics listed below were also applied to all of our activities and initiatives.
| Investment Theme | Strategic Priority | Objective |
|---|---|---|
| Healthy Developmental Trajectories | Developmental Origins of Health and Disease through the Lifespan | Prevent non-communicable diseases by understanding how environmental exposures from conception through to early childhood impact later life disease |
| Preterm Birth | Improve care and outcomes for babies born preterm and support new avenues of research into causes and consequences of preterm birth | |
| Healthy Reproduction, Pregnancy, Childhood and Youth | Environmental Health | Understand how the physical, social and physiological environment influences reproductive, fetal, child and youth health |
| Healthy Pregnancy | Ensure healthy pregnancy and birth including a greater understanding of fertility and infertility | |
| Healthy Public Policy and Systems Integration | Integrated Child & Youth Research and Health Services | Optimize the Canadian pediatric health care system through better integration of services across multiple jurisdictions and across the life course. |
| Mental Health | Improve mental health outcomes for children and youth through prevention and early diagnosis, increased access to services, and effective treatments. | |
| Enabling Tactics | Capacity Building | Support a healthy and vibrant research community capable of addressing our strategic priorities to improve health outcomes |
| Knowledge Translation | Ensure research evidence is used to improve health | |
| Partnerships and Collaboration | Build local, national and international partnerships to support our community and learn from the knowledge and wisdom of others | |
| Data Sharing | Ensure collaborative, robust, and easily accessible data for evidence-informed decisions | |
| Global Health | Embrace global health to inform strategic initiatives |
IHDCYH in Numbers
Funds committed to IHDCYH initiatives:
- $150.4M from CIHR + $54.6M Partner contributions = $205.0M
- 29 initiatives
- 112 funding opportunities
- 629 grants
- 22 Community consultations
- 11 Researcher workshops
- 10 Knowledge translation and media events
- 9 Capacity building workshops
- 1 National mandate-wide conference
Funding in IHDCYH Mandate Area
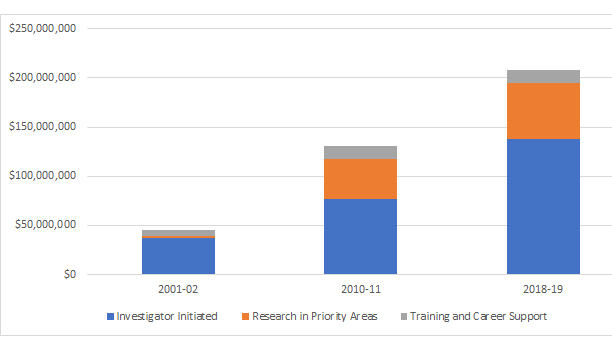
Figure 1 - Long description
| 2001-02 | 2010-11 | 2018-19 | |
|---|---|---|---|
| Investigator Initiated | $37,149,985 | $76,448,205 | $137,497,700 |
| Research in Priority Areas | $2,422,918 | $40,611,822 | $56,785,793 |
| Training and Career Support | $5,855,957 | $13,483,811 | $13,919,311 |
Researchers funded in IHDCYH's mandate
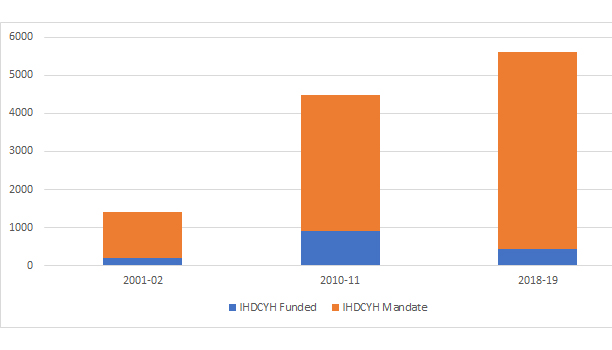
Figure 2 - Long description
| 2001-02 | 2010-11 | 2018-19 | |
|---|---|---|---|
| IHDCYH Funded | 199 | 907 | 431 |
| CIHR funded | 1012 | 2663 | 4761 |
Healthy Developmental Trajectories
Initiative introduction: Preventing chronic disease from the beginning of life
Funds committed: $42.9M
The Healthy Life Trajectories Initiative (HeLTI) is addressing non-communicable diseases (NCDs), including cardiovascular diseases, respiratory diseases, diabetes and mental health challenges, which are responsible for 60% of deaths globally with 80% of those deaths occurring in low- and middle-income countries.
HeLTI is a 10-year, international research effort developed in partnership with funders from Canada, India, China and South Africa. The initiative aims to impact global policy and reduce incidence of NCDs worldwide by investigating how the environment and an individual’s genetics interact during conception, fetal life, infancy and early childhood to affect the development of NCDs later in life. This concept is referred to as the Developmental Origins of Health and Disease or DOHaD.
Through this initiative, researchers will identify and apply evidence-based interventions early in life that will have lasting positive impacts on health, especially if applied at the national policy level on a global scale. HeLTI has been rolled out through 3 broad approaches.
- Canadian Interdisciplinary DOHaD Teams: building capacity and making new discoveries
- Linked International Intervention Cohorts: Improving population health from pre-conception onwards
- Canadian DOHaD Cohort Registry: Optimizing use of existing data and facilitating collaboration
Partners:
- CIHR-IHDCYH, CIHR-IIPH, CIHR-IA, CIHR-ICRH, CIHR-IGH, CIHR-IPPH
- World Health Organization (WHO)
- National Natural Science Foundation of China
- Department of Biotechnology of India
- Medical Research Council of South Africa
Supporting healthy beginnings in four countries
Timeline: 2017 - 2027
The HeLTI Linked International Intervention Cohorts (LIICS) are a unique research collaboration between Canada, China, India, South Africa and the World Health Organization (WHO) that is supporting research teams that are establishing a DOHaD-based ‘intervention’ cohort in each of the four countries.
The LIICs are using an innovative funding model, with the funding agencies from each country remaining closely engaged through a HeLTI Council that provides oversight. This approach also includesa HeLTI Office that has supported the development of a cutting-edge international governance structure to enhance harmonization of the cohorts and data sharing opportunities, and a WHO Secretariat to provide monitoring and technical support, and maximize the opportunity for global impact.
Each cohort has a lead researcher from Canada and a lead researcher from the participating country. All four teams are targeting measures of obesity, as well as additional indicators of body composition, glucose metabolism, blood pressure and child development. Each team will use prospective interventions tailored to the communities they are working with, such as nutritional supplementation, parental social support, hygiene and infection prevention, and obesity prevention. The four cohorts are also all aligned through common data collection, management and analysis processes, along with shared key principles to maximize collaboration, data sharing and capacity building. The overall goal is to decrease obesity, improve metabolic health, and improve child development, leading to a decrease in life-time chronic disease. The cohorts have begun enrolling participants at pre-conception, will soon begin implementing their interventions, and will follow the participants’ outcomes through pregnancy, infancy and into childhood.
Teams:
- TROPHIC Trial – 2 provinces in Canada
- Cindy-Lee Dennis, St. Michael’s Hospital (Toronto, Canada) and Catherine Birken, Hospital for Sick Children (Toronto, Canada)
- BUKHALI Trial – Soweto, South Africa
- Stephen Lye, Sinai Health System (Toronto, Canada) and Shane Norris, University of the Witwatersrand (Johannesburg, South Africa)
- EINSTEIN Study – Mysore, India
- Stephen Matthews, Sinai Health System (Toronto, Canada) and Kumaran Kalyanaraman, KEM Hospital (Pune, India)
- Life Tree Study – Shanghai and Shijiazhuang, China
- William Fraser, Université de Sherbrooke (Sherbrooke, Quebec) and Hefeng Huang, Shanghai Jiao Tong University (Shanghai, China)
Key facts:
- 10 years
- 175 centres
- 22,000 women
- 10,000 pregnancies
Understanding the developmental origins of health and disease
Timeline: 2016 - 2021
The goal of the Canadian Interdisciplinary DOHaD Teams is to improve health through an increased understanding of how biological, social and environmental exposures impact human health and development.
Each team brings together basic scientists with social scientists. By supporting these multi-disciplinary teams, CIHR is building capacity in the DOHaD field. In addition, the teams are encouraged to consider the ultimate policy implications of their research.
“New relationships with public health, and community health care workers and the public have resulted in a robust knowledge translation program and outreach efforts”
Deciphering the metabolic signatures of the metabolic syndrome (MetS) in young children
Sonia Anand, McMaster University
Dr. Anand and her team are researching the risk factors that underlie the development of “metabolic syndrome”, which is a group of conditions including increased blood pressure, excess abdominal fat and high blood sugar. Development of metabolic syndrome leads to a higher risk of diabetes and heart disease. The team’s goal is to uncover markers in the blood of pregnant women and their children (from birth through 5 years), that reflect dietary intake and can forecast a child's likelihood of developing metabolic syndrome. Their work will help to strengthen the scientific evidence supporting dietary guidelines for pregnancy and early childhood and have direct relevance for clinical practice and public health policy for the prevention of diabetes and heart disease.
The effects of paternal environmental exposures on offspring development and health
Sarah Kimmins, McGill University
Dr. Kimmins and her team are focussed on understanding fertility in men and how the father’s environment (diet, BMI & toxicants) impacts the sperm, clinical outcomes, development of embryos and offspring health. The paternal sperm epigenome has been implicated in diseases in children such cancer, diabetes, schizophrenia and autism. The team has identified specific epigenomic signatures associated with fertility, embryo development and disease in sperm from men exposed to toxicants, or who have an elevated BMI. They are now working to determine if environmental-induced damage to the sperm epigenome can be prevented or reversed through education and health-based intervention strategies.
Prenatal programming of children's mental health: Epigenetic mechanisms and resilience promotion
Michael Kobor, University of British Columbia
Dr. Kobor and his team are identifying whether multiple sources of stress during pregnancy predict biological markers in the offspring and whether those markers predict children's mental health early in life. The study focuses on CANDLE (Conditions Affecting Neurocognitive Development and Learning in Early childhood), a birth cohort with rich biological, demographic, environmental and health data from 1,500 mother and child pairs. The research team aims to identify maternal stress factors that affect gene regulation and mental health in children, as well as prenatal and postnatal protective factors that can be targeted to promote resilience to later life disease. This information will then be used to develop targeted interventions to improve mental health in high-risk children, families and communities.
HUGS for HEALTH: Healthy Bugs for Healthy Babies DOHaD Team
Deborah M Sloboda, McMaster University
Dr. Sloboda and her team are working in animal and human studies to uncover molecular mechanisms that regulate relationships between adiposity, pregnancy weight gain and the maternal gut bacteria that mediate the early origins of childhood obesity. Before and during pregnancy, regulating weight gain may be one way to mediate maternal obesity-induced non-communicable disease risk, to improve both maternal pregnancy conditions and the fetal environment. Using a participatory research approach, the team has used their empirical evidence and new knowledge gained in experimental studies, to inform a community-based knowledge transfer and work program of intervention, that aims to improve diet and body composition of women before and after conception.
Effects of environmental, genetic and maternal factors on child and youth psychopathology
Ashley Wazana, Jewish General Hospital (Montreal)
Dr. Wazana and his team are examining how prenatal depression, genetic susceptibility and early maternal care, including maternal attunement and sensitivity, interact to explain the development of depression in early childhood and adolescence. This research project is an international collaboration across four comparable longitudinal projects, MAVAN, GEN-R, ALSPAC and GUSTO. A key impact of this project is the development of a prediction model for psychopathology early in childhood which in turn advances treatment outcomes. This model has the potential to improve health and health care through early identification, prevention, and intervention which will reduce the risk and severity of psychopathology in adolescence and later in life.
Research Profile
Babies and Bacteria
Dr. Deborah Sloboda and her Canadian Interdisciplinary DOHaD Team are using multiple techniques to explore the link between maternal obesity and excess weight gain during pregnancy and increasing childhood obesity rates.
One element of her research program is the Mothers to Babies (M2B) Study, where the team is using community outreach activities to connect with community care providers, public health organizations, pregnant women and new moms and look at the knowledge, experiences, barriers and supports related to nutrition and health during pregnancy. The aim is to transfer knowledge about the health benefits of improving early life environments to those who can create appropriate policies and programs to support the needs of women and their families.
Dr. Sloboda and her team have identified a wide range of barriers and issues influencing diet and health during pregnancy, as well as intervention strategies to initiate positive change. These influences span not only immediate impacts on eating habits, but also social and environmental factors that impact nutritional status.
In combination with their work in the community, the team is studying how the relationships between the maternal gut bacteria, adiposity and pregnancy weight gain mediate the early origins of childhood obesity and chronic disease. By understanding the biological pathways that regulate gut health and immunity in pregnancy, particularly when there is excess adiposity, it is possible to design nutritional interventions for use during pregnancy that would reduce risks for chronic health issues in the child.
“By providing supports to enable good health before and during pregnancy, we’re helping women, their babies and their extended families, for many generations to come.”
Increasing the use of existing data in DOHaD research
Timeline: 2016 - 2021
The Canadian DOHaD Cohort Registry was funded to serve as a national resource for large, cross-cohort studies in the DOHaD field.
Canada is internationally recognized for its high-quality, population-based cohorts and databases that collect data and biological samples to support innovative research and inform the development of social, environmental and health policies. However, many Canadian cohorts remain under-exploited, and individual studies often do not have the statistical power, specific data items or appropriate design needed to be of broader use and to fully support increasingly complex research questions. As a consequence, existing data is being under-utilized and opportunities for collaboration are being lost. Cohort registries offer the ability to share data across cohorts.
Research Advancement through Cohort Cataloguing and Harmonization (ReACH)
Isabel Fortier, Research Institute of the McGill University Health Centre
The ReACH initiative, led by Dr. Isabel Fortier in collaboration with Drs Stephanie Atkinson, Alan Bocking and William Fraser, has developed a database of metadata and definitions of variables from 25 longitudinal Canadian DOHaD cohorts. This database provides a valuable resource for researchers in the DOHaD field as it can be used to identify data from multiple cohorts that can be linked to facilitate larger and better powered studies. ReACH also provides a harmonization platform, data analysis tools, open source software and technical support that can be used to harmonize, integrate and co-analyse data.
“We are providing the research community with the means to optimize usage of existing data and samples as well as facilitate the establishment of research collaboration. By providing these resources, we hope to advance science and propel the use of research results to improve human health.”
Key facts:
- 25 Canadian pregnancy and birth cohorts
- 53,300 mother-child pairs
- 17,800 fathers
- 17 research areas
- 132 categories
- 95,500 variables
Initiative introduction: Helping preterm infants survive and thrive
Funds committed: $10.8M
The Preterm Birth Initiative is using multiple approaches to address the negative impact of being born preterm.
In Canada, preterm birth accounts for nearly two thirds of infant deaths and is associated with increased morbidity throughout the life course and subsequent chronic disease. In addition to these health effects, preterm birth has social and financial impacts on the affected individuals and their families, and places additional costs on society in terms of healthcare and education.
The Preterm Birth Initiative was informed by a consultation with stakeholders in preterm birth and related fields and is supporting work to: 1) Improve care practices and infant outcomes through the application of research evidence (Preterm Birth Network), 2) Test new and innovative ideas in preterm birth research (Catalyst Grants), and 3) Identify and implement improvements to the overall perinatal health care systems (Perinatal Health Care Systems Improvement Team).
Improving care and outcomes for preterm infants across Canada
Timeline: 2016 - 2021
The overall aim of the Preterm Birth Network is to break down the traditional silos of obstetrics, perinatal, neonatal and developmental care, and bring together clinicians and researchers together to improve the outcomes of infants born preterm.
Bringing the different groups together in a network focused on producing research evidence will support the integration of research across the continuum of preterm birth from pregnancy through to early childhood. A particular focus of the network is to conduct research into improving the quality of clinical care and effectively implementing evidence-based practice changes on a national scale to improve outcomes.
Improving Outcomes for Preterm Infants and their Families: A Canadian Collaborative Network
Prakeshkumar Shah, Sinai Health System (Toronto)
Dr. Shah and his team have united researchers, obstetricians, neonatologists, pediatricians, nurses and families across Canada in an effort to increase the rate of preterm infant survival without complications by 30% over 5 years.
To date, the network has developed a database that collects maternal, paternal, neonatal and infant information on all preterm infants born at less than 29 weeks gestation at level III NICUs across Canada. The network is taking a patient-oriented approach and is guided by a steering committee that includes 2 parents and a parent advisory group that includes 27 parents from participating institutions. Seven research projects are ongoing within the network and the network is also developing new methods of cost analysis to estimate the economic burden of preterm birth and monitor the economic impact of improving outcomes. Early impacts include demonstrating that administration of magnesium sulphate during pregnancy is neuroprotective in growth restricted fetuses. Using evidence to improve care practices just before and immediately after birth has been shown to be associated with reduction of mortality and/or severe neurological injury for infants born at less than 29 weeks gestation. Implementation of a practice called deferred cord clamping, was also associated with reduction of mortality and severe neurological injury.
Blue sky ideas in preterm birth research
Timeline: 2016 - 2018
The objective of the Catalyzing Innovation in Preterm Birth Research funding is to generate new and innovative ideas in preterm birth research.
The funded researchers are investigating a range of topics from prevention and prediction of preterm birth, through approaches to improving care, to following up on the impact of integrating parents into the care of their infant in the Neonatal Intensive Care Unit (NICU). The projects have resulted in scientific discovery and peer-reviewed articles. These grants have catalyzed innovative and ongoing investigation to advance our knowledge in preterm birth research.
Impact of Family Integrated Care on child developmental health, maternal psychosocial distress and health system costs at 18 months corrected age
Karen Benzies, University of Calgary
Alberta has the highest preterm birth rate of the Canadian provinces. The majority of preterm babies are admitted to a Level II neonatal intensive care unit (NICU), a highly technological environment where parents have historically had limited involvement in the care of their baby. Dr. Benzies and her team are testing the use of Alberta Family Integrated Care©™ (FICare) in NICUs across the province. This psycho-educational intervention integrates and involves parents in the NICU by sequentially building their knowledge, skill, and confidence so they are well-prepared to care for their preterm baby before discharge. If the team finds that Alberta FICare©™ improves outcomes for preterm babies and their parents, the intervention will be implemented in all Level II NICUs in Alberta.
Biostatistical methods for estimating the cumulative impact of environmental contaminant exposures on preterm birth
Lawrence McCandless, Simon Fraser University
A growing body of research points to the role of environmental pollution and toxic chemicals as a possible cause of adverse pregnancy outcomes including preterm birth. Dr. McCandless is leading a team of epidemiologists and biostatisticians that is examining the effects of toxic environmental chemicals on preterm birth. They have developed several novel statistical methods to measure the health impacts of environmental chemical exposures in pregnancy, particularly with regards to biomarkers, and are using these techniques to analyse data from birth cohort studies. This work is contributing to Canada’s leadership in perinatal epidemiology research and our understanding of the role of environmental pollution in preterm birth.
Control of expiration in the newborn period
Silvia Pagliardini, University of Alberta
Newborn preterm infants often display irregular breathing during sleep, which can be life-threatening or cause life-long health consequences if not properly managed. Dr. Pagliardini and her team are investigating how active expiration (forcefully breathing out) and the recruitment of expiratory muscles contribute to breathing during sleep. As a first step, the team investigated breathing, expiration and sleep in rats. Building on this work, the team moved onto investigating expiration across sleep states in human infants to determine if enhanced expiratory activity ameliorates breathing. They are also investigating the correlation between expiration and improved respiratory function across sleep cycles in term and preterm infants, and in patients affected by sleep disordered breathing. This work will build the foundation to develop new treatment approaches for sleep disordered breathing in infants.
Understanding the unique health-protecting properties of the infant microbiome
Katherine Ryan, University of British Columbia
Humans are host to an enormous number of microorganisms called the “microbiome”, which plays a critical role in helping digest food and prevent infection. Infants and adults have very different microbiomes due in part to dietary differences. For instance, bacteria that commonly populate the infant gut have developed the ability to survive by digesting unique carbohydrates present only in human breast milk, giving these bacteria a selective advantage over other gut bacteria that cannot digest such carbohydrates. As recent research suggests that these bacteria may protect babies from diseases, Dr. Ryan and her team are employing approaches from biochemistry, microbiology, and chemistry to better understand these unique infant-associated bacteria.
Magnetic Resonance Imaging (MRI) of the cervix to predict spontaneous preterm birth
Oksana Shynlova, Sinai Health System (Toronto)
Pregnancy involves an intimate physiological interaction between mother and child. The gatekeeper of pregnancy is the uterine cervix. In a normal pregnancy, the cervix softens and dilates to facilitate the delivery process. Cervical incompetency or early dilation is thought to lead to preterm birth. Dr. Shynlova and her team are improving our understanding of cervix physiology during pregnancy using techniques such as magnetic resonance imaging (MRI), histological staining and gene expression analysis. The team has discovered that the uterine cervix possesses a sphincter-like property that may prevent premature delivery and that may weaken or disappear as pregnancy advances leading to preterm birth. They have demonstrated that cervical MRIs may help predict the imminence of preterm birth in high-risk patients, thereby opening the door to new therapeutic strategies to improve cervical integrity in pregnancy.
Development of therapeutics for prevention and treatment of pre-eclampsia: One of the leading causes of preterm birth in Canada
Graeme Smith, Kingston General Hospital and Queen’s University, Kingston
Pre-eclampsia is a condition that develops during pregnancy, and is marked by problems with blood vessels and blood pressure, which can cause significant problems for the mother and baby. Dr. Smith and his team are developing novel approaches to prevent and treat pre-eclampsia by increasing external exposure to carbon monoxide (CO) during pregnancy or increasing the body’s production of CO. They have shown that inhaled CO increases dilation of blood vessels, which improves blood flow. They have also identified molecules that increase CO production in the body – and particularly the placenta blood vessels. The team has completed exploratory studies showing the potential for these molecules as dietary supplements that could be tested in the prevention or treatment of pre-eclampsia.
Research Profile
Developing a method to predict preterm birth
Pregnancy is a complex process that relies on intricate coordination between the fetal membranes surrounding the baby, and different parts of the uterus including the uterine muscle, lining, uterine neck, and cervix. In a healthy pregnancy, at around week 40, the uterus contracts, the membranes break, the cervix becomes extremely soft and then dilates to allow for the birth of the baby.
Each year in Canada approximately 30,000 or 8% of infants are born preterm – at less than 37 weeks of gestation. Infants born preterm can spend months in the neonatal intensive care unit, and are at an increased risk of death as well as both short- and long-term health problems.
There is currently no way to identify women who will deliver preterm, and there are no effective treatments for women who are at high risk of a preterm birth – identified on the basis of having previously delivered one or more babies preterm.
To find a method to predict preterm birth, Dr. Oksana Shynlova, who was awarded a CIHR-IHDCYH Preterm Birth Catalyst Grant, is working to address critical questions about how the cervix changes during term and preterm birth. She is using animal models, biological markers and imaging tools, such as magnetic resonance imaging (MRI), to study the cervix in pregnant women who are at risk of having a preterm birth.
“We are aiming to identify the link between structural changes in the cervix and the readiness for delivery,” says Dr. Shynlova. ”In pregnant mice, we have discovered that changes to the top part of the cervix are associated with preterm birth. We are now working to determine if similar changes to the cervix of high-risk pregnant women can predict preterm birth.”
This research may lead to an effective way to predict preterm birth and test therapeutic approaches to preventing early delivery in high-risk women who have already delivered a preterm baby.
Enhancing health systems for perinatal care
Timeline: 2017 - 2022
The Perinatal Health Care Systems Improvement Team aims to address the significant variability in maternal and infant outcomes, perinatal care practices, and health care system performance between provinces.
Although Canada has an excellent system of perinatal care overall, gaps exist that have led to suboptimal processes and disparities. These problems create challenges for health care professionals and prevent the delivery of high-quality care to mothers and their infants. The team, led by Dr. KS Joseph, is developing, implementing and evaluating evidence-based recommendations to improve the perinatal health care system on a national level.
A systems approach for enhancing perinatal care regionalization
KS Joseph, University of British Columbia
Dr. Joseph and his team of 70 investigators are analyzing the structure, processes and outcomes of the perinatal health care system across Canada to determine what is working well and where improvement is needed. Using data from the Canadian Institute for Health Information, as well as provincial and territorial heath systems data, the team is identifying how perinatal care is provided across the country – from small hospitals in rural areas to the most advanced specialist hospitals. They are looking at the different levels of care provided, emergency transport, access to care and health outcomes of mothers and babies. “Our overall objective is to ensure that mothers and babies receive a level of care that is appropriate to level of risk they face,” says Dr. Joseph.
As of February 2020, the team had completed their analysis of adverse outcomes among mothers and babies and compiled 7 reports identifying provinces, levels of care and hospitals with high rates of adverse outcomes. The reports examine adverse outcomes following a first caesarean delivery, in subsequent pregnancies following a previous caesarean delivery, associated with forceps delivery and vacuum delivery, related to transport issues, and associated with the transfer of low and high-risk women before delivery or after delivery. These reports will be sent to provincial/territorial ministries of health, reproductive care programs and hospitals with the aim of catalyzing efforts to address these high adverse outcome rates through better organization and delivery of health services for pregnant women and newborns.
The team has support and collaboration from numerous professional organizations including the Society of Obstetricians and Gynaecologists of Canada, the Public Health Agency of Canada, the Canadian Perinatal Programs Coalition and the Canadian Paediatric Society.
Healthy Reproduction, Pregnancy, Childhood and Youth
Initiative introduction: Understanding the impact of the environment on health
Funds committed: $18.5M
The CIHR Environments and Health Signature Initiative (EHSI) is supporting research focused on understanding how the environment effects human health, enhancing data sources and methods for environmental health research, and understanding how to prevent and mitigate environmental threats to health.
Both our natural and built environments contain many synthetic and naturally occurring chemical and biological agents, some of which may be harmful to health. To prevent and avoid human exposure to potentially harmful agents, society needs sound information and ways to address both exposure and hazards across the continuum that exists from source, to exposure, to biological effect, to individual response, and ultimately to public health impact. EHSI is made up of 3 funding opportunities: Environments, Genes and Chronic Disease, Environmental Urban Health Research Consortium and Intersectoral Prevention Research . The Initiative is co-led by the Institutes of Population and Public Health and Infection and Immunity in partnership with IHDCYH and the Institutes of Circulatory and Respiratory Health; Nutrition, Metabolism and Diabetes; Gender and Health; Aging; and Indigenous Peoples Health.
Identifying how the environment, our microbiome and epigenetics are all linked to disease
Timeline: 2016 - 2021
The objective of the programmatic grants in Environments, Genes and Chronic Disease is to advance our understanding of how environment-gene interactions and environment-microbiome-gene interactions affect the development of chronic non-communicable disease, disease patterns and human health across the life course.
A range of projects were funded, five of which are looking at family, child and youth health, including work on paediatric obesity, inflammatory bowel disease, endocrine disrupting chemicals and asthma.
The developmental origins of obesity and obesity-related complications in children
Vernon Dolinsky, University of Manitoba
Dr. Dolinsky and his team are tackling the rise of obesity and type 2 diabetes in children – particularly First Nations children for whom the risk of these health conditions is higher than in other children. They are taking advantage of the growing evidence that epigenetic effects during fetal development and environmental exposures during early life can program the risk for obesity and cardiometabolic disease. Their research program aims to understand the interaction between our genes and environmental exposure during pregnancy through identifying metabolites and DNA methylation patterns that are characteristic of childhood disease.
Endocrine disrupting chemicals: Towards responsible replacement
Barbara Hales, McGill University
Dr. Hales and her team are focused on ensuring that safe alternatives replace endocrine disrupting chemicals, such as brominated flame retardants, phthalate plasticizers and bisphenol A. Restrictions on the use of these chemicals have led to their replacement with alternatives. However, there are no requirements for manufacturers to demonstrate that the alternatives are safer than the chemicals they replace. Dr. Hales and her team, which includes researchers from Canada, United States, Europe and South Africa are determining the extent to which endocrine disrupting chemicals and their alternatives are present in food, water and breast milk. They have developed a platform to screen these chemicals for bioactivity and are working with partners to develop a framework for the responsible assessment of replacement chemicals.
The diet-microbiota-gut axis in pediatric inflammatory bowel disease
Alain Stintzi, University of Ottawa
Dr. Stintzi is leading an interdisciplinary research program focused on investigating the complex interactions between diet, the gut microbiota and the host, and characterizing the role of microbial food-derived metabolites in the pathogenesis of inflammatory bowel disease (IBD). IBD is a chronic, relapsing, inflammatory disorder of the gastrointestinal tract that includes Crohn’s disease and ulcerative colitis. IBD is thought to occur in genetically susceptible individuals who suffer from a weakened intestinal barrier, maladaptive immune responses and microbial imbalance. Evidence suggests that environmental factors, including diet and sunlight exposure also affect the development of the disease. Dr. Stintzi and his team are testing the hypothesis that a disruption of the food-microbiota-host interface leads to IBD or promotes disease chronicity.
Gene and environment effects on lung health and risk for chronic respiratory disease, asthma & COPD
Padmaja Subbarao, University of Toronto
Dr. Subbarao and her team are focused on improving the understanding of the impact of nutrition, home and outdoor environmental exposures and the interaction of viruses, the microbiome and genetic factors on lung growth in infancy and early childhood. It is known that poor lung function in early life can be a risk factor for the development of chronic lung symptoms and can be the result of chronic respiratory diseases such as asthma and COPD. The knowledge they generate will inform the development of novel targets to alter the trajectory of poor lung growth and respiratory symptoms in children.
Understanding how modifiable environmental factors interact with the genome in the development of asthma
Stuart Turvey, University of British Columbia
Asthma is the most common and burdensome chronic non-communicable disease affecting young Canadians. Dr. Turvey and his team are working to determine how key modifiable environmental factors interact with the genome in the development of asthma in children and youth. They have focused on four environmental factors, specifically: breastfeeding, gut microbiome, traffic-related air pollution and urban natural spaces, and community and family psychosocial environments. By identifying and addressing gaps that will lead to the generation, translation and mobilization of new knowledge about childhood asthma, the team will take a major step towards better understanding the interplay of environment and genetics in the development of this prevalent chronic disease.
Linking environmental data to health data to create new knowledge in urban health
Timeline: 2016 - 2021
The aim of the Canadian Environmental Urban Health Research Consortium grant is to create a data hub and methodological hub that enables environmental researchers to collaborate with health and other relevant researchers as well as data experts to improve measurement, modeling and analysis of health and environmental data as it relates to urban areas.
Having access to comprehensive environmental data and well-developed methods is key to understanding the impact of the environment on health. However, sources of social and environmental data relevant to health are disparate and difficult to access. This collaboration is enabling knowledge users to take full advantage of existing data to prevent and mitigate health risks, as well as enhance positive health effects of the urban environment across the life course.
The Canadian Environmental Urban Health Research Consortium (CANUE)
Jeffrey Brook, University of Toronto
CANUE is furthering our understanding of how to design and modify cities to improve, not degrade, population health. The key to this work is linking standardized environmental exposure data about air quality, green spaces, walkability, noise and other aspects of the urban/suburban environment to existing human health data platforms. This includes incorporating cohorts focusing on reproductive, fetal and/or child health. By bringing together expertise from academia, government, NGOs and the private sector and collaborating with similar initiatives around the world, CANUE is developing standard measures of environmental factors. This work gives environmental health researchers a remarkable opportunity to uncover how these factors create both positive and negative impacts on health.
Key facts:
- 275+ researchers and students
- 250+ unique variables
- 13 research areas
- 120+ data requests per year
- $2.2M of additional funding for projects
Reducing harmful exposure and promoting healthy environments
Timeline: 2016 - 2021
The programmatic grants in Intersectoral Prevention Research aim to address the need for research on the ongoing environmental effects on human health and development of effective health promotion and disease prevention strategies.
A range of projects were funded, including three that are examining the effects of the built and industrial environment on child and youth physical and mental health.
The built environment and active transportation safety in children and youth
Brent Hagel, University of Calgary
Dr. Hagel and his team are studying how the built environment can promote active transportation, including walking and bicycling, among children and youth while protecting their safety. At the same time, they are examining the health and health equity impacts of built environment strategies in Canadian urban centres. They have developed engagement strategies to enhance intersectoral action and initiated cross-jurisdictional research to inform solutions to the issue of low child and adolescent participation in active transportation. Overall, their research program will provide the evidence base for recommendations to ensure safer environments for active transportation.
Patterns of resilience among youth in contexts of petrochemical production and consumption in the global north and global south – the RYSE project
Michael Ungar, Dalhousie University
Both oil and gas production and the process of consumption have large impacts, both positive and negative, on social, economic and environmental systems that affect young people’s mental health and overall wellbeing. Dr. Ungar and his team are seeking to better understand these complex relationships at both ends of the carbon cycle to study the resilience of young people and the systems with which they interact. The team represents a multidisciplinary and multisectoral group of researchers and community and industry partners in Alberta, Canada and South Africa. The team’s findings will inform socially and environmentally sound government policies and industry practices.
Initiative introduction: Preventing and treating disease by understanding how the microbiome impacts health
Funds committed: $17.2M
The Canadian Microbiome Initiative 2: A Focus on Function and Translation Research is supporting research to enable the development of preventive and therapeutic interventions through a deeper understanding of the microbiome’s role in human health.
Over the past decade, technological advances have enabled the study of the microbiome at various sites on the body. These studies have shown that the microbiome is associated with a variety of human diseases such as asthma, anxiety, autism, malnutrition, obesity and rheumatoid arthritis. Research is shifting from descriptive and correlational studies, to studies that address the causational links between the microbiome and human health. Advancing this research offers tremendous potential for new therapeutic approaches.
The Canadian Microbiome Initiative 2 is building on previous investments and Canada’s research strengths, to invest in research that addresses this opportunity through two elements – a Research Core and Research Teams. The initiative is led by the CIHR Institutes of Infection and Immunity; Nutrition, Metabolism and Diabetes; Genetics; and Gender and Health in collaboration with IHDCYH and the Institutes of Aging; Cancer Research; and Neurosciences, Mental Health and Addiction. Funding partners on the initiative include JDRF Canada and Mitacs.
Providing resources and support to microbiome research in Canada
Timeline: 2018 - 2023
The Canadian Microbiome Initiative 2: Research Core is acting as a resource to the Canadian microbiome research community and to the Canadian Microbiome Initiative 2 Research Teams.
The Research Core serves a number of functions including facilitating sharing of expertise, knowledge and resources; supporting the integration of sex- and gender-based analysis and ethical considerations in research related to the microbiome and human health; and promoting the translation of research outcomes into improved health, social and economic benefits for Canadians, including both preventative and therapeutic interventions. The Research Core is also working to facilitate the addition of microbiome samples to existing large cohorts in Canada. These shared resources will help to foster and standardize microbiome research across Canada.
IMPACTT: A microbiome research core based on Integrated Microbiome Platforms for Advancing Causation Testing and Translation
Kathy McCoy, University of Calgary
The Integrated Microbiome Platforms for Advancing Causation Testing and Translation (IMPACTT) is a
multi-centre collaboration that is fostering and standardizing microbiome research across Canada. The new gnotobiotic facility at the University of Calgary is able to support the study of complex functional interactions between the microbiome and the host. IMPACTT is facilitating microbiome studies in human cohorts by providing expertise for study design, sample collection and computational analysis. The IMPACTT team is also establishing and maintaining a large repository of microbes, with genetic and metabolic information to enable functional microbiome studies. Finally, the team is developing a platform to discover links between microbial genes, proteins, and metabolism with microbial function, and then further link this to human health and disease.
Understanding how the microbiome influences health and disease
Timeline: 2019 - 2024
The Canadian Microbiome Initiative 2: Research Teams are developing new knowledge on the causational roles of the microbiome in human health and disease, which will lead to the development of new preventative and therapeutic interventions.
Health research areas being investigated by the teams include childhood asthma, cervical cancer, diabetes, youth inflammatory bowel disease and maternal malnutrition.
Microbiome-asthma linkage in preterm infants
Marie C Arrieta Mendez, University of Calgary
The lungs are among the organs most affected by premature birth. In Canada and globally, premature infants are more likely to develop recurrent wheeze than term infants. Until now, it was accepted that this condition was the result of lung damage caused by medical practices needed to support respiration. However, epidemiological evidence shows that infants who do not develop lung damage are nevertheless at increased risk of asthma. Recent findings implicate the large community of microbes in the human gut as a factor that contributes to asthma. Dr. Arrieta Mendez and her research team will be the first to unravel microbiome-asthma linkages in the highly vulnerable premature infant population with the aim of identifying microbiome-based approaches to treatment.
The microbiome in cervical cancer
Adam Burgener, University of Manitoba
Cervical cancer is one of the most common cancers in women. The presence of high-risk human papillomavirus (HPV) is a widely known cause of cervical cancer, and women who are living with HIV are particularly vulnerable to this disease. Recent evidence suggests that the bacterial communities that live within the vagina are important for the clearance of HPV and the development of cervical cancer. Dr. Burgener and his research team are studying the vaginal microbiome in women who have HPV infection and evaluating the properties of vaginal bacteria with advanced molecular techniques to determine what role they play in disease. The team hopes to identify microbial targets for treating women with HPV to prevent or inhibit progression to disease.
Dissecting host-microbiome modifiers of type 2 diabetes risk
André Marette, Université Laval
The global epidemic of obesity and type 2 diabetes (T2D) reduces lifespan and quality of life, and exerts enormous pressure on the health system. Changes in the composition of the gut microbiota are known to accompany obesity and factors that increase risk of T2D. Dr. Marette and his team have already shown that bacteria and bacterial fragments are altered in the upper gut and that they selectively accumulate in the circulation, liver and the fat deposits of obese women and men. The team is now working to define the identity and function of the specific bacterial strains compartmentalized in specific gut segments versus body tissues in the progression of insulin resistance and T2D. This knowledge may help develop novel diagnostic, preventive and therapeutic approaches for diabetes.
The impact of pathogen-microbiome dynamics on maternal nutrition during pregnancy in young women
John Parkinson, Hospital for Sick Children (Toronto)
Maternal and child undernutrition are global problems with important consequences for survival, incidence of acute and chronic diseases, healthy development and economic productivity. Aside from dietary deficiencies, the gut microbiome is increasingly viewed as playing a critical role in nutritional status. To understand the links between maternal nutrition, birth outcomes and the gut microbiome, Dr. Parkinson and his team are studying changes in microbiome communities in two groups of young women – one in Pakistan, one in Canada – over the course of their pregnancy. Understanding these complex relationships and their impact on malnutrition and birth outcomes, will improve diagnoses and inform the development of novel targeted interventions that can significantly improve maternal health and child development.
Causational roles of the gut microbiome in childhood asthma: Leveraging the CHILD Cohort Study
Padmaja Subbarao, Hospital for Sick Children (Toronto)
Asthma is a lung disease that makes it hard to breathe. The CHILD Cohort Study, which involves nearly 3500 babies and their families, was set up to investigate why some children develop asthma, and find out how we can prevent it from starting. Scientists working on the CHILD data have discovered that gut bacteria are important in helping our immune systems develop properly so that we do not get asthma. Dr. Subbarao and her team are using new technologies to find out how gut bacteria are causing or preventing asthma. This information will lead to new ways to prevent and treat asthma by using or targeting gut bacteria.
Role of microbes in the pathogenesis of pediatric inflammatory bowel diseases: From discovery, through causation, to novel treatments
Bruce A Vallance, University of British Columbia
Inflammatory bowel diseases (IBD) are chronic conditions that damage the intestines and cause lifelong pain. Current drug treatments, which focus on suppressing the immune system, are not always effective and carry risks. Dr. Vallance and his team have found several types of unusual bacteria in patients with IBD. These bacteria invade cells in the gut, are recognized by the immune system and trigger inflammation. The findings suggest that these “pathobiont” bacteria may cause or aggravate IBD. By investigating different approaches to removing these harmful bacteria from the gut, the research team is aiming to discover novel ways to treat children with IBD.
Microbiome regulation of beta-cell autoimmunity and type 1 diabetes
Jayne S Danska, Hospital for Sick Children (Toronto)
Type 1 diabetes (T1D) is caused by autoimmune inflammation of the pancreatic islets and destruction of the beta cells – the cells that make insulin. The rise in T1D over the past several decades suggests that environmental factors play a role in the disease. The complex bacterial community in the intestines is essential for metabolism and the development and function of our immune system. Dr. Danska and her team are working to understand how environmental changes have influenced the gut microbiome in infants with a genetic risk for T1D. The team is studying the microbes in the infant gut and identifying the immune responses in children at risk for diabetes. This work will support new therapeutic strategies for preventing and treating new onset T1D.
Supporting the new generation of clinician-investigators in obstetrics and maternal-fetal medicine
Funds committed: $7.5M
Timeline: 2016 - 2021
The Clinician-Investigator Teams in Obstetrics and Maternal-Fetal Medicine (C-I Teams) program is providing early and mid-career researchers who are also practicing clinicians with the resources they need to establish teams that will increase their research capacity.
There is a remarkable opportunity cost and disincentive for clinicians in the field of Obstetrics and Maternal Fetal Medicine to do research, with very few clinicians having access to adequate protected time and resources. Consequently, most of the active researchers in obstetrics and maternal-fetal medicine in Canada today are late career, with very few early- and mid-career investigators. The C-I Teams program is addressing this issue by funding five teams led by early- and mid-career investigators who are focusing on aspects of research related to healthy pregnancy including non-communicable diseases such as obesity, prematurity and pregnancy complications in high risk pregnancies.
DOH-Net: The Diabetes, Obesity and Hypertension in Pregnancy Research Network
Howard Berger, St. Michael’s Hospital, Toronto, ON; Nir Melamed Sunnybrook Research Institute, Toronto, ON; Beth Murray-Davis, McMaster University, Hamilton, ON
Drs Berger, Melamed, and Murray-Davis are leading the Diabetes, Obesity and Hypertension in Pregnancy Research Network (DOH-Net), a multi-disciplinary research program of obstetrical, midwifery and maternal-fetal medicine specialists. This network is filling critical knowledge gaps and working to optimize the management of diabetes, obesity and hypertension in pregnancy. Researchers in the network have found that, in Ontario, more than 1 in 6 pregnancies are affected by obesity, 1 in 100 pregnancies by pre-pregnancy diabetes or hypertension and more than half of women gain weight in excess of what is recommended. These conditions magnify the risk of preterm birth, abnormal fetal growth and newborn complications.
Montreal Emerging Research Team in Maternal Fetal Medicine (MERe)
Isabelle Boucoiran, Ariane Godbout, Catherine Taillefer, and Sandrine Wavrant, Université de Montréal, Montréal, QC
Drs Boucoiran, Godbout, Taillefer, and Wavrant are committed to enhancing the capacity of hospitals within the Université de Montréal network to deliver health care services to women from conception to the neonatal period. They have developed a platform that facilitates research projects involving early-career maternal fetal medicine clinicians and local fundamental research teams and that enables rapid integration of the results into clinic practice. The platform also supports the creation of provincial, national and international partnerships for knowledge translation.
Collaborative Obesity in Pregnancy Research Group: Supporting a team to investigate placental adaptations to obesity
Barbra de Vrijer and Genevieve Eastabrook, University of Western Ontario, London, ON
In London, Ontario, 45% of births are in overweight or obese mothers. This situation poses significant challenges when it comes assessing the risk and preventing placenta-related diseases, such as stillbirth, fetal growth restriction and preeclampsia. Drs de Vrijer and Eastabrook are leading the Collaborative Obesity in Pregnancy Research Team, which is developing new clinical tools to predict and diagnose obesity-related chronic inflammation, cardiovascular and metabolic stress that is believed to underlie these pregnancy complications. The team is using novel technologies such as metabolomics and pulse wave analysis to assess vascular stiffness and MRI to investigate fetal adipose tissue development.
RIGHT CARE in the RIGHT PLACE at the RIGHT TIME: Maternity care provision in women who conceive using assisted reproductive technologies or are obese
Laura Gaudet, Ottawa Hospital Research Institute, Ottawa, ON, and Maria Vélez, Queen’s University, Kingston, ON
Drs Gaudet and Vélez are focused on identifying knowledge and evidence gaps in maternity care for pregnant women who are obese or pregnant via assisted reproductive technologies (ART). The team will use this new knowledge to develop a care map and screening tools to triage these women to the most appropriate maternity care providers. They have carried out several systematic reviews and determined the predictors of adverse pregnancy outcomes in obese pregnant women or women pregnant via ART. They are now identifying the most important risk factors and using those to develop a tool to triage women that will be tested in a clinical trial.
Clinician Scientist Team on Prematurity
Jean Charles Pasquier, Haim Abenhaim, and Anne-Marie Côté, Université de Sherbrooke, Sherbrooke, QC
Drs Pasquier, Abenhaim, and Côté and their team are seeking to better understand the causes of prematurity so that pregnant women may be offered tailored treatments to prevent preterm delivery and the potentially serious consequences for the newborn baby. The team is studying a treatment approach to prevent premature labour involving the use of a pessary and progesterone. They are also evaluating a urine test to predict preeclampsia, and validating a method to better classify the different causes of preterm birth and assess their impact on the health of the newborn.
Key facts:
- 111 journal articles
- 36 invited presentation
- 100 conference presentations
- 30 new grants as PI
Healthy Public Policy and Systems Integration
Building Canada’s research capabilities in health services and policy research
Funds committed: $5.5M
Timeline: 2012 - 2017
The Applied Chairs in Reproductive, Child and Youth Health Services and Policy Research program was developed to build capacity in applied health services and policy research and to bridge the gap between researchers, decision makers and other knowledge users, particularly in the domain of reproductive, child and youth health.
“The Applied Chair award was critical to my research career and supported a large number of trainees who now form a critical mass of child and youth health services researchers primarily within departments of paediatrics in Canada.” (Funded researcher)
The program provided support to mid-career faculty (5-15 years’ experience) who were conducting reproductive, child and youth health services and policy research; and dedicated to working with decision makers to frame their research questions and interpret their results, as well as train and mentor students, fellows, junior faculty and others seeking career opportunities in the field. The program was developed and launched by IHDCYH Scientific Director Dr. Michael Kramer and his team in 2011 and came to fruition during Dr. Shoo Lee’s term as Scientific Director.
The Applied Chairs program was very successful and produced a large body of high-impact research that has changed health services and policy in Canada including new concussion legislation in Ontario; improvements to Canadian perinatal health surveillance; comparison of neonatal outcomes and findings on how to improve care practices in 11 countries; and collaboration with youth and their families to give them a voice and engage them in working to improve the health care services they receive. The program also built significant capacity in reproductive, child and youth health services and policy research across Canada including establishing the careers of a large number of independent researchers in this area.
Evidence-informed health services delivery for Canadian children and youth
Astrid Guttmann, Hospital for Sick Children and Institute for Clinical Evaluative Sciences
Dr. Guttmann conducted policy-relevant research to evaluate current health system reform strategies in Ontario that aim to improve access to and coordination of services for children and youth with chronic health and mental health conditions.
Highlights:
- Developed ‘Scorecard for Mental Health of Children and Youth in Ontario’ in partnership with Ministries of Health, Education, and (former) Children and Youth Services to evaluate mental health services in Ontario
- Research on epidemiology and costs of concussion in children and youth informed new legislation in Ontario – Rowan’s Law (co-led with Dr. Alison Macpherson)
- Built community by co-founding maternal and child health theme group within Canadian Association for Health Services and Policy Research (CAHSPR)
Health services research for optimizing maternal, fetal and infant health
KS Joseph, University of British Columbia
Quality control and cost containment are the key public health imperatives for ensuring a sustainable health care system and for improving the health of Canadians. Along with colleagues in perinatology, health services and health policy, Dr. Joseph conducted research in maternal, fetal and infant health to enrich the scientific knowledge base for making informed decisions regarding quality control and cost containment issues.
Highlights:
- Identified reasons for rising stillbirth rate in Canada and worked with Perinatal Services BC, Statistics Canada and the Public Health Agency of Canada to improve ongoing perinatal surveillance
- Worked with Society of Obstetricians and Gynaecologists of Canada to develop confidential enquiry process for maternal deaths
- Awarded two prizes by obstetrics and gynaecology journals for best article in 2017 and most highly cited in 2013
Bridging the gaps between evidence, policy and injury prevention
Alison Macpherson, York University
Dr. Macpherson’s research aimed to better understand policies related to the prevention of childhood injuries. She worked with policy-makers, researchers and non-profit organizations to promote evidence-based policies related to children’s safety.
Highlights:
- Worked with 2 Indigenous communities engaging youth in storytelling and developed YouTube videos around safe and unsafe places in their communities
- Partnered with the City of Toronto to conduct an observational study of children in playgrounds that may lead to policy changes regarding playground design and surfacing
- Served as the Co-Editor in Chief of the revised textbook for the Canadian Injury Prevention Curriculum used to educate public health nurses and practitioners in injury prevention
Maternal and Perinatal Placental Ethnicity Development (MAPPED) program: A policy-directed clinical research program to attain healthy mothers and health newborns in Canada
Joel Ray, St. Michael’s Hospital (Toronto)
Dr. Ray studied outcomes arising in pregnancy, around the time of delivery and after delivery to identify modifiable or actionable factors that can be used to evaluate the impact of policy and practice changes. His research projects used linked administrative health databases and retrospective population-based serial cross-sectional studies.
Highlights:
- Evaluated risk factors for pre-eclampsia and developed practical preventive approach using aspirin
- Developed ethnicity-specific neonatal weight charts for male and female infants born to mothers from different world regions
- Assessed safety of MRI use during first trimester of pregnancy
- Identified long-term risk factors for cardiovascular disease associated with pregnancy
International Network for Evaluation of Outcomes (iNeo) of neonates: A quality improvement project via collaborative comparison of international health services for neonatal care
Prakesh Shah, Mount Sinai Hospital (Toronto)
Dr. Shah established an international network that compares outcomes, practices and non-tangible environmental, physical and human factors between countries and neonatal units to identify the best possible practices to improve outcomes of very low birth weight infants in Canada and globally. Through collaborative learning, the participating countries are developing and applying best practice strategies that incorporate local context and culminate in improved patient-oriented and disease-oriented outcomes via refined health service delivery.
Highlights:
- Established international network of 11 countries called iNeo that includes 393 neonatal units to compare neonatal care practices and outcomes as a means to improve quality of NICU care in all participating countries
- Collected data on >200,000 very preterm infants and conducted epidemiological studies evaluating outcomes, variations and trends
- Surveyed >320 neonatal units worldwide to learn about variations in practices, healthcare service delivery and environmental factors including support services for parents
- The network continues to expand and build on their international data collection, harmonization and dissemination efforts to examine whether differences in practices, service delivery and environment are associated with specific infant outcomes
A child and youth centered approach to applied health services and policy research
Roberta Woodgate, University of Manitoba
Dr. Woodgate conducted innovative applied health services and policy research that involves health system managers, policy makers and healthcare providers, as well as children and youth who are directly impacted by the research. She focused on three priority areas of study: 1) children and youth living with chronic physical and mental illness; 2) children and youth living with disabilities and complex health needs; and 3) promoting health and access to health care for children and youth.
Highlights:
- Developed innovative methodological approaches to empowering young people and their families as key actors in understanding and improving the services and policies affecting them
- Identified an important gap in literature and practice related to self-harm among youth and received further funding to undertake research with international partners to explore school-based interventions that promote mental health and wellbeing
- Received additional funding to evaluate an enhanced telemental health services model to improve mental healthcare services and outcomes for youth living in First Nations communities
Key facts:
- 39 new independent researchers
- 49 fellows and junior faculty
- 150 PhD, MSc and BSc students
- 17 policy changes
- 102 media articles
- 236 presentations
- 477 peer reviewed journal articles
Initiative introduction: Improving the delivery of primary healthcare in Canada
Funds committed: $19M
The Community-Based Primary Health Care (CBPHC) Signature Initiativesupports highly innovative approaches to improving the delivery of appropriate and high-quality community-based primary health care to Canadians.
The Initiative is co-led by the CIHR Institute of Health Services and Policy Research and Institute of Population and Public Health in collaboration with several partners including IHDCYH. IHDCYH provided support to two main components, the CBPHC Innovation Teams and the pan-Canadian SPOR Network in Primary and Integrated Health Care Innovations (SPOR PIHCI).
Sparking innovation in primary healthcare research
Timeline: 2013 - 2018
The CBPHC Innovation Teams were designed to improve primary healthcare by supporting creativity and collaboration among the various healthcare stakeholders.
The objectives of the CBPHC Innovation Teams were to develop, evaluate and scale-up successful models of community-based primary healthcare across Canada that targeted prevention and management of chronic disease, reduction of inequities in access and outcomes in vulnerable population, and optimization of outcomes in specific populations, for example, pregnant women, children and youth. To foster the innovative approaches needed to achieve these objectives, the Innovation Teams were comprised of an inter-professional mix of investigators, health professional scientists, and clinicians who were advised by patients, families, and communities and supported by senior decision makers.
Barriers and facilitators in access to child and youth mental health services
Richard Audas, Memorial University of Newfoundland
Children and youth with mental health and oppositional behavioural problems and their caregivers are among the most vulnerable members of Canadian society. Their conditions are complex and require an interdisciplinary and inter-sectoral approach to provide treatment and care. In their program of research, Dr. Audas and his team focused on three highly prevalent conditions: Autism Spectrum Disorder (ASD), Conduct Disorder and Eating Disorders. The project team included, primary health care physicians, policy makers and researchers from across Atlantic Canada who compared the experiences and outcomes of individuals across four different jurisdictions. Their objective was to develop best practice guidelines and tools for primary health care physicians to facilitate better management and outcomes of this vulnerable population. In addition to achieving this objective, the team brought together key stakeholders and decision makers around the issue of addressing child and youth mental health; conducted a needs assessment and produced a report for the Autism Society of NL; produced numerous publications and conference presentations; and shared their findings through interviews.
The TRANSFORMATION Study: Transforming community-based primary health care through comprehensive performance measurement and reporting
Sabrina Wong, University of British Columbia
Although Canada has made substantial financial investments in renewing community-based primary health care over the last decade, there has been no way to routinely capture whether efforts improve community-based primary health care or quality of care have been effective until now. Through their research program, Drs Wong, Johnston, Burge and their team developed an innovative approach to primary health care performance measurement and reporting that is relevant and credible to patients, clinicians and decision-makers. They have developed patient experience surveys, reporting mechanisms, and practice-based data collection methodologies which will give Canadians more equitable care with better population outcomes at reduced cost. The TRANSFORMATION Team has also piloted an automated survey system for collecting patient experience data – a cost-effective and innovative ‘first’ in Canada.
Building networks; building on our strengths in primary healthcare
Timeline: 2014 - 2020
The Strategy for Patient Oriented Research Network in Primary and Integrated Healthcare Innovations (SPOR-PIHCI) is a network of networks that builds on regional and national assets in community-based primary and integrated health care.
SPOR is a CIHR research strategy that was developed in partnership with provinces and territories, philanthropic organizations, academic institutions, and health charities with the aim of making patient-oriented research a reality in Canada. To date, SPOR has funded a wide variety of patient-oriented research through two mechanisms: SPOR Networks and Innovative Clinical Trials.
The SPOR PIHCI networks are working together to develop, evaluate and scale up new approaches to the way in which care is provided and coordinated by multiple health care providers, including nurses, social workers, pharmacists, dietitians, public health practitioners, physicians and others in a range of community settings including people’s homes, healthcare clinics, physicians’ offices, public health units, hospices, and workplaces. The focus of the work is on individuals with complex health needs where integration of care across multiple services is critical to improve the patient experience and outcomes. A range of work in child and youth health was funded including several provincial networks engaged in developing, evaluating and scaling up new approaches, as well as projects looking at specific aspects of the delivery of integrated services for families, children and youth.
“Our study is one of the first cross-provincial comparisons of [diabetes care] transition practices in [youth] in Canada. We also got to explore the work different types of providers currently do and the potential role they could play in the care of young adults with diabetes. It is the type of important and difficult work that would not have happened without the support of CIHR and IHDCYH.”
SPOR PIHCI Projects
Variations in how youth with type 1 diabetes transition into adult care
Roger Chafe, Memorial University of Newfoundland and Labrador
Dr. Chafe and his team are helping improve outcomes and the overall patient experience for youth adults with type 1 diabetes as they make the transition from pediatric to adult care. The team examined the transition practices and outcomes for young adults with diabetes in two Canadian provinces: Ontario and Newfoundland and Labrador. The team found significant variation between and within both provinces and generally poor outcomes for patients in the years after they turn 18. They used their findings to help develop a transition clinic and found that, if correctly supported, family physicians can help make transition into adult care a positive experience for youth with diabetes.
Building cross-generational wellness and resilience in multi-generational Indigenous households: A scoping review
Cheryl Currie, University of Lethbridge (Alberta)
The Canadian Aboriginal residential school system has adversely affected parenting skills and the success of many Indigenous families. These cross-generational experiences have been compounded by a lack of adequate housing in Indigenous communities. As a result, service providers face the challenge of working with families struggling with significant levels of psychological trauma living in overcrowded, multi generational homes. Service providers have identified key barriers in their work to assist these families including a lack of access to research on models and strategies they can use to work in a more effective, integrated way. The purpose of this scoping review was to map integrated service delivery models and strategies that agencies can use to support Indigenous households struggling with psychological trauma. Findings aimed to summarize national and international models that agencies can use to integrate and embed supports to address mental health and social well-being throughout a household, so that all individuals can heal and support each other as they strive toward their personal goals.
Children with complex health conditions: Let's learn who they are and their needs to better serve them!
Shelley Doucet, University of New Brunswick
Dr. Shelley Doucet, Dr. Rima Azar, and Dr. William Montelpare aim to improve services and programs available to children experiencing complex health conditions. They developed NaviCare/SoinsNavi as a result of the needs assessment phase conducted by the team in 2015 to 2016, which involved over 120 interviews with children/youth and their families as well as with health, social, and educational stakeholders. Through NaviCare/SoinsNavi, children are assigned patient navigators who help families coordinate access to appropriate services and resources for their children. Navigators helps facilitate more convenient and integrated care to support the physical, mental, emotional, and social needs of the children and their families. This important resource has already helped 200 families across New Brunswick.
Policies and program innovations that connect primary health care, social services, public health and community supports in Canada: A comparative policy analysis
Jeannie Haggerty, McGill University
CPPPHC (Comparing Policies and Programs of Primary Health Care) is a Pan-Canadian comparative study of programs in Canadian Provinces that aims to connect primary health care, social services, public health and community supports to one another to ensure continuity and quality of care for patients with complex care needs. Patients include both community-dwelling older adults (65+) experiencing functional decline and children and youth (0-25) with high functional needs. This work aims to provide policy makers, national health policy bodies, and health researchers with key contextual information in each Canadian province regarding where provinces are in terms of “realizing Primary Health Care”, as Western countries increasingly recognize the necessity of using a multi-service integrated approach to ensure continuity of care for patients with complex care needs.
Case management in primary care to improve outcomes among frequent users of health care services with chronic conditions: A realist synthesis of what works, for whom and in what circumstances
Catherine Hudon, Université de Sherbrooke
Dr. Hudon studies case management intervention for patients with chronic diseases and complex care needs in primary care clinics across Canada. By identifying the facilitators and barriers of case management implementation in clinics, understanding the relationships between the actors, contextual factors, mechanisms and outcomes of the case management intervention, and identifying the next steps towards case managed spread in primary care, they aim to inform local practices and policies and contribute to improve the health of patients with complex healthcare needs who frequently use healthcare services. Ultimately, this will increase the performance of healthcare systems and specifically mitigate ineffective use and costs.
Creation of a Comprehensive Health Profile of Children in New Brunswick and Prince Edward Island and Development of Intra-Provincial Population-Based Birth Cohorts
Carole Tranchant, Université de Moncton (New Brunswick)
Previous research suggests that exposure to adverse environments early in life, including the prenatal period, is associated with later adult health outcomes such as obesity, diabetes, cardiovascular disease and mental health conditions. In Canada, the Maritime provinces experience a higher prevalence of obesity and chronic diseases compared to other provinces. Dr. Tranchant’s project aimed to identify and evaluate selected administrative datasets from New Brunswick (NB) and Prince Edward Island (PEI) to create two intra-provincial health profiles of 18-month-old children and likewise to establish the foundation for a birth cohort database in each province using existing datasets. The outcomes from this innovative research aimed to yield important insights into children's health status and trajectory that can be used toward chronic disease prevention to reduce the needs for complex care later in life. The NB and PEI child health profiles and the future birth cohort databases will allow various stakeholders and knowledge users to monitor and report on child health over the long term, and to evaluate current practices and future health interventions to establish well-informed and effective primary prevention strategies.
Research Profile
New Brunswick patient-navigation centre helps children and youth with complex care needs and their families
Caring for a child can be overwhelming at the best of times but this only multiplies when that child has complex care needs. Parents and caregivers may experience added stress as they try to navigate what can be a very complicated system of health and social services.
Dr. Shelley Doucet at the University of New Brunswick and Dr. Rima Azar at Mount Allison University created NaviCare/SoinsNavi to help parents and caregivers in New Brunswick navigate the services available for children and youth with complex care needs. This research- based centre operates with funding from the New Brunswick Children’s Foundation.
Patient navigators at NaviCare/SoinsNavi provide a free, bilingual service for families. They also serve care providers by helping them identify services and programs available to their patients.
Since opening, the centre has served over 120 families, including Hannah McGee and her son Jackson who was born prematurely. He weighed just one pound, ten ounces at birth and spent more than 100 days in the neo-natal intensive care unit. A patient navigator has helped Hannah not only locate but also finance specialized care for little Jackson.
NaviCare/SoinsNavi is also living laboratory where Dr. Doucet and Dr. Azar, along with research associate Dr. Alison Luke, oversee the evaluation of services, conduct research and supervise clinical and research trainees. The research has been supported with grants from the Canadian Institutes of Health Research and the New Brunswick Health Research Foundation.
Since we started, we’ve been carrying out an ongoing evaluation. The information we’re collecting is helping to identify barriers and gaps in services.
Follow NaviCare/SoinsNavi on Twitter: @NaviCareNB
Initiative introduction: Improving the experience and outcomes of patients as they experience health care transitions
Funds committed: $6.6M
The Transitions in Care initiative is a multi-Institute initiative that aims to improve the health and wellness of Canadians by supporting research that transforms the health system to optimize the outcomes of individuals experiencing transitions in care.
Co-led by the Institutes of Circulatory and Respiratory Health; Health Services and Policy Research; Indigenous People’s Health and IHDCYH, in partnership with the Institutes of Aging; Cancer Research; Gender and Health; Musculoskeletal Health and Arthritis; Neurosciences, Mental Health and Addiction; and the Strategy for Patient-Oriented Research, the initiative focuses activity on transitions in care that occur across the life trajectory, that accompany changes in health status or care, and that impact populations vulnerable to adverse outcomes, including seniors, Indigenous Peoples, LGBTQ individuals, new immigrants and people living in rural or remote locations.
The Transitions in Care initiative is made up of several components and IHDCYH is providing support to the Best and Wise Practices grants, Team grants and Evaluation grants. Within these components, IHDCYH has funded projects that focus on transitions in care that affect pregnant women, children and youth.
Identifying best practices for effective transitions in care
Timeline: 2019 - 2020
The Transitions in Care Best and Wise Practices grants support planning and information sharing activities, partnership development as well as evidence gathering to facilitate the collection of data and build relevant research capacity.
Pregnant women, children and youth who enter the health care system may experience transitions in care such as moving from one professional to another, from hospital to home care or from a child to adult healthcare setting. These transitions, if not successful, can lead to poor health outcomes. The Best and Wise Practices grants are providing development funds to groups that are gathering additional evidence and building partnerships to address challenges, gaps and barriers to mitigating negative outcomes resulting from care transitions.
Uncovering gaps in diabetes management during transitions in care amongst members of the Métis Nation of Alberta: a two-eyed seeing approach
Kelsey Bradburn, Métis Nation of Alberta
Approximately 3 million Canadians, or 8.1% of the population are living with diagnosed diabetes representing a significant health burden on Canadians. Indigenous Peoples (First Nations, Inuit, and Métis) are more likely to experience diabetes than non-Indigenous Peoples and can face considerable barriers when attempting to access the care needed to best manage their health. Through her research, Dr. Bradburn and her team are identifying gaps in diabetes management among members and from the perspective of the Métis Nation of Alberta to gain a better understand life with a chronic health condition and to develop strategies that may improve outcomes during transitions in care.
Identification and prioritization of transitional care interventions for adolescents and young adults with childhood onset disabilities
Sarah Munce, University Health Network (Toronto)
Transition from the child to adult health care system is a complex process that should include a variety of services. If the transition to the adult health care system is not successful, it can lead to poor health outcomes and decreased opportunities to participate in the community. Without appropriate services, health problems may go unnoticed, putting adolescents and young adults at risk of developing even more health problems. There is a lack of training related to aging with a childhood onset disability among adult health care providers. This results in a growing population of youth with disabilities who receive no care at all in the adult health care system. To address these concerns, Dr. Munce and her team are collaborating with decisions makers, experts, and consumers to determine the impact of transitional care interventions on the quality of life and transitional care outcomes among young adults with childhood onset disabilities.
A mixed method community action study exploring 'life-cycle' healthcare transitions with Canadians experiencing intersex variations
Caroline Sanders, University of Northern British Columbia
Intersex variations are variations in sex characteristics (genitals, hormones, chromosomes, reproductive organs) which vary from the established norms for 'male' and 'female'. Between 0.05 and 4% of the population has intersex variation, with some variations being as common as twins or red hair. Most variations are natural and healthy, but they can influence physical appearance, function, fertility and sexual wellbeing. To better understand current health care practices at times of transition and to set research priorities, Drs Sanders and Todd and their team are exploring the health care experiences of Canadians with intersex variations. Their research will help to identify health care practices that promote lifelong well-being for this community.
PED-UCATE - Pediatric Emergency Department Use of Communication Technologies to Activate Transitions Home Effectively
Lori Wozney, IWK Health Centre (Halifax)
In 2016 to 2017, over 2.4 million children and youth under the age of 19 visited an emergency department [ED] for care in Canada with the majority (87%) being discharged to their home residence. Many of these patients require some form of continued care once they are home. When discharged, caregivers need to be provided with the necessary knowledge and skills to effectively manage their child's care to avoid negative health impacts and outcomes and unnecessary return visits to the ED. Drs Wozney and Curran and their team are studying the use of information communication technologies such as computer kiosks, apps, interactive whiteboards to improve the discharge process and the transition from hospital to home for children and youth who visit pediatric emergency departments.
Evaluating existing initiatives to improve transitions in care
Timeline: 2019 - 2021
The Transitions in Care Evaluation Grants will support the rigorous evaluation of the effectiveness, appropriateness and impact of activities already implemented to improve transitions in care.
To optimize the outcomes for patients experiencing transitions in care, it is critical to understand the effectiveness of interventions, tools, practices, policies, technologies and programs that are already in place. Through the 2-year Evaluation Grants, researchers and knowledge users are formally evaluating transitions in care activities including transitions from hospital to home care for children with medical complexity, mental health care transitions for youth and transition from pediatric to adult care settings for youth with chronic conditions.
The evaluation of the Connected Care Program for children with medical complexity: A prospective cohort study with embedded health economic and qualitative analysis
Reshma Amin, Hospital for Sick Children (Toronto)
In Canada, there are a growing number of children who are living longer than before due to new medical technologies such as a feeding tubes and breathing machines. Some of these supports can be used outside of the hospital setting, allowing patients and their families to return to their homes sooner. However, the care received during this transition period from hospital to home is not well coordinated and often results in frequent return visits to hospital placing added stress on patients and their families. In 2018, the Ontario Ministry of Health funded the Connected Care Program to assist children with medical complexity and their families make the transition from hospital to home or community care. Dr. Amin and her team are evaluating Ontario’s Connected Care Program to determine the effect on visits to the emergency department, the experience of patients and families, the costs on the healthcare system and the experience of healthcare providers.
Facilitating effective mental health care transitions for youth: Evaluation of the transition support worker model
Kristin Cleverley, University of Toronto
Transitions out of hospital child and adolescent acute mental health services (CAMHS) to the community or adult mental health services (AMHS) remain a serious health system issue in Canada. We know that about half of youth drop out of care during this critical developmental and service transition. Lack of care as well as poorly planned discharges lead to worse mental health, unnecessary health costs and increased use of correctional and social services. Transition support worker programs exist across Ontario and Canada to facilitate the complex transitions out of hospital-based CAMHS care. Drs Cleverley, Shime, McCann and their team are evaluating the use of transition support workers as a model for facilitating the effective transition of children and adolescents from acute mental health services to community or adult mental health care services and for ensuring continuity of care.
U-Flourish student mental health research: Transitions to mental health care
Anne Duffy, Queen’s University (Kingston, Ontario)
The demand for student mental health care is increasing and threatening to overwhelm resources across university campuses. However, there is limited data to inform universities about how best to support the mental health of an increasingly diverse student population, identify those at highest risk and facilitate the timely transition to appropriate mental health care. To gain a better understanding of how to provide effective mental health services, Dr. Duffy and her team are studying the transition to mental health care among university undergraduate students. They are assessing the relationship between access to mental health services, mental health and academic success.
Evaluating the impact of a navigation service for transitional-aged youth with mental health and/or addictions concerns and their families
Anthony Levitt, Sunnybrook Research Institute (Toronto, Ontario)
Transitional-aged youth with mental health and/or addictions concerns often fall through gaps between care settings and systems, which can negatively impact their long-term outcomes. Many transitional-aged youth may also have family members involved in their care, yet their families might not know where to turn for support in finding the best resources for the youth and for themselves, when needed. There needs to be more support for transitional-aged youth with mental health and/or addictions concerns and their families leading up to, during, and after care transitions. The Family Navigation Project is a service in which navigators work one-on-one with transitional-aged youth between the ages of 13 and 26 with mental health and/or addictions concerns and their families to help them find their way through the health care system and get connected to the right care. Dr. Levitt and his team are evaluating this service to understand the benefits for clients, their families and the healthcare system.
Evaluating the impact of primary care patient-provider relationships on Emergency Department utilization by adolescents with chronic conditions
Susan Samuel, University of Calgary
Traditionally, primary care has focused on establishing long-standing patient-physician relationships to providing coordinated, continuous, patient-centered and comprehensive care. Yet, it is unknown whether adolescents and young adults with chronic conditions maintain relationships with primary care providers when they transfer from specialized pediatric to adult-oriented care. To address this knowledge gap, Dr. Samuel and her team are studying the relationship between youth with chronic health conditions and their primary care providers through the transition from pediatric to adult care. The knowledge will be used to facilitate stronger linkages between specialty pediatric care, mental health care and primary care, and to inform transition policies and practices for young adults with chronic conditions.
Implementing evidence-based practices to optimize transitions in care
Timeline: 2019 - 2023
The Transitions in Care Team Grants are supporting the implementation of health, health system and health care activities that optimize transitions in care.
The Team Grants are being rolled out in two phases to support activities that are ready to be implemented now and those that need additional development and evaluation. The second phase of Team Grants will also support activities that may be developed through the Best and Wise, Evaluation, and/or the first phase. Grants in the first phase were funded in 2019.
A virtual transition intervention for children and adults transitioning to home ventilation in Ontario: A pragmatic randomized controlled trial
Reshma Amin, Hospital for Sick Children (Toronto)
The number of people that use a ventilator at home is increasing in Canada and around the world. These individuals have complex health problems. Unfortunately, the care for individuals using mechanical ventilators isn't coordinated, which results in frequent visits to the hospital and stress on the patient and family. Virtual care is a way to improve healthcare for individuals using ventilators because it can bring "the right people with the right expertise at the right time" into the homes of these complex patients. The newly developed virtual care platform called a TouchAway™ is sophisticated enough to meet the care needs of individuals using ventilators. Dr. Amin and her team are studying the use of this virtual platform to support the care of children and adults who use ventilators at home. The study will determine the effect on visits to the emergency department, the experience of patients, families, and healthcare providers and the costs on the healthcare system.
Facilitating transitions and access across the pregnancy continuum of care: A health system intervention for Indigenous women living in northern Manitoba
Patricia Gregory, Red River College (Winnipeg, Manitoba)
Pregnancy is a time of transition. Women and families transition from pregnancy, to birth to post pregnancy care. Each transition requires a connection to various health care providers, from a nurse, physician or midwife, sometimes to a specialist, and from care in an office setting, to hospital care for birth and back home. In northern Manitoba one of every three pregnant women does not receive adequate care in pregnancy. Indigenous women and children experience the greatest health inequities in this region and in Canada more broadly. These inequities are compounded by transitions between health care systems. The federal government provides health care in First Nations communities, however, for specialized services and birth, women need to transition to the provincial health care system. Many barriers including, travel, transportation issues, financial constraints, poor communication, different providers and weak referral links are encountered through those transitions. To address these concerns, Dr. Gregory and her team are examining a pregnancy collective impact network of service providers, families and community members led by a patient navigator to determine if this approach helps improve the continuity of care and reduces health inequities for pregnant Indigenous women.
ED to EPI: Using SMS (text) messaging to improve the transition from the emergency department to early psychosis intervention for young people with psychosis
Nicole Kozloff, Centre for Addiction and Mental Health (Toronto)
Psychosis, a syndrome characterized by loss of touch with reality, is a disabling and life-threatening condition that typically starts in adolescence and young adulthood, a time of life associated with gaps in mental health service use. Despite the availability of effective treatment through early psychosis intervention programs, around half of youth do not access these services. Even when youth with psychosis present in crisis to the emergency department, rates of follow-up care are poor, in large part related to young people not attending early psychosis intervention services when they are referred. To address this issue, Dr. Kozloff and her team are studying the use of text messages as way of improving the transition of youth with psychosis from the emergency department to an early psychosis intervention program. This study will provide evidence on what would be a low-cost, easily implemented strategy for getting more young people with psychosis appropriate treatment earlier, leading to improved long-term trajectories.
The impact of an innovative ehealth transition intervention on self-management skills among young adults with congenital heart disease
Andrew Mackie, University of Alberta
There have been major advances in the care of children born with heart defects (congenital heart disease) over the past 3 decades. Now over 90% of children with congenital heart disease reach adulthood. However, adolescent and young adult "survivors" are at risk of further heart problems. Unfortunately, most have very little understanding of their congenital heart disease and they lack confidence communicating with doctors and nurses about their heart. Over half do not attend specialized adult congenital heart disease clinics after graduating from their children's hospital, despite being advised to do so. This increases the risk that new heart problems, which may develop in early adulthood, will be discovered too late. Nurse-led programs to help with transition are effective but time-consuming, expensive and not easily accessible to adolescents living in rural communities. Dr. Mackie and his team are working to determine whether a smart phone app is more effective than a nurse-led program to help young adults with congenital heart disease transition to adult care while improving their knowledge of their heart condition and self-management skills.
Keeping in Touch (KiT) with young adults as they transition through type 1 diabetes care
Rayzel Shulman, Hospital for Sick Children (Toronto)
For young adults living with type 1 diabetes, moving from pediatric to adult care can be overwhelming because many feel unprepared and find it difficult to make a meaningful connection with the new adult team. It is also challenging for young adults to balance their diabetes self-care with other competing priorities such as education, social activities and work, putting them at risk for life-threatening complications and poor diabetes control. Many young people find it challenging to attend diabetes clinics, but there are other ways to improve the connectedness between young people and their pediatric and adult diabetes teams. Dr. Shulman and her team are evaluating the impact of a mobile ehealth application on the lives of young adults with type 1 diabetes as they transition from pediatric to adult care and on the connection between young adults with type 1 diabetes and their adult care team.
Neurosurgical Transition e-Program (Neuro-STEP): Pilot evaluation of an e-Health program to improve the transition of neurosurgical patients from remote locations to specialist neurosurgical care, across life's trajectory from pediatric to adult, and through dynamic changes in acute or chronic health states.
Gelareh Zadeh, University Health Network (Toronto)
Currently, long wait-times for patients to see a specialist are a big problem. For neurosurgery patients any delay in seeing a specialist can result in anxiety and worse outcomes. Some people travel from long distances to see a neurosurgeon. Others are neurosurgery patients who have been used to the pediatric setting and now must transition to an adult hospital. Finally, after having had a neurosurgical operation, an individual could either be going home, a local hospital or to rehabilitation. In any of these scenarios, it is helpful to have real-time information customized to the specific person, diagnosis and state of health. Dr. Zadeh and her team have developed an internet-based platform with an ehealth company that will help manage specialist referrals and transitions in care and provide patients with real-time information on their diagnosis and the status of their referral. The team will test the application with a group of neurology patients evaluate its effectiveness based on the satisfaction of patients and referring physicians as well as wait-times and administrative costs.
Promoting child health through a streamlined ethics review
Funds committed: $2.5M
Timeline: 2020 - 2025
The initiative to Promote Child Health Research through a Collaborative Approach to a Streamlined Ethics Review or Pediatric REB Initiative will enable the development of research support infrastructure, to facilitate the ethics review process thereby enhancing and expediting pediatric research.
Investigators developing multi-site research studies in Canada often encounter challenges with gaining Research Ethics Board (REB) approval, in particular across more than one province. This can delay the research, increasing the costs and timelines of conducting projects that are often publicly funded. These challenges can discourage clinician-researchers from undertaking important child health research and reduces the ability of Canadian researchers to compete and participate in the international research arena.
The Pediatric REB Initiative was developed in response to these challenges in consultation with stakeholders from each of the Children’s hospitals and research institutes across Canada, as well as Health Canada and provincial health agencies. The $2.5M in funding provided through this initiative by IHDCYH and the Institute of Genetics will enable the development of research support infrastructure to facilitate multi-site studies for enhanced and expedited pediatric research. This will increase our preparedness to respond swiftly to emerging health threats, while improving the care provided to one of the most important populations in Canada, our children.
Canadian Collaboration for Child Health: Efficiency and Excellence in the Ethics Review of Research (CHEER)
Richard Carpentier, Susan Marlin, Thierry Lacaze-Masmonteil; Clinical Trials Ontario (CTO) and the Maternal Infant Child & Youth Research Network (MICYRN)
Led by Drs Marlin, Carpentier and Lacaze-Masmonteil, in partnership with over 35 experts in research ethics review and child health from across Canada, the CHEER team is building a web-based system that researchers and REBs across the country can use to manage a single REB review. “Streamlined research ethics approval plays a key role in conducting successful, efficient clinical research”, says Susan Marlin, President and CEO of Clinical Trials Ontario. “We are thrilled to be working with MICYRN and colleagues from across this country to advance child health research in Canada.”
The CHEER team will also be working with researchers and REBs to develop educational and other materials to ensure research involving children has the highest ethical standards. “Development of an effective education component is key to ensuring research teams, trainees, and REB members are informed of new systems and processes in a timely manner,” says Thierry Lacaze-Masmonteil, Scientific Director of MICYRN. “Through all phases of the project, we will engage researchers, sub-speciality networks, and patients and their families to ensure information that can help improve child health in Canada is delivered in an accessible format.”
This initiative provides a key piece of research support infrastructure, with huge potential to provide an invaluable opportunity for health research in Canada and contribute to maintaining our research community at the forefront of international efforts.
Improving technologies and practices to identify, treat and prevent brain injury
Funds committed: $6.3M
Timeline: 2013 - 2018
The Traumatic Brain Injury Initiative was funded to develop new technologies and best practices for identifying and treating mild traumatic brain injury.
The initiative was led by the Institute of Neurosciences, Mental Health and Addiction (INMHA) in partnership with IHDCYH, Fonds de recherche du Québec – Santé (FRQS), the Hotchkiss Brain Institute and the Ontario Neurotrauma Foundation. Through a series of catalyst grants and team grants, the initiative supported research into developing new technologies and best practices for treating mild traumatic brain injury in children and youth, as well as adults impacted by blast injuries. The topics studied include developing better tools for diagnosis; improving consensus on diagnosis and treatment approaches; reducing the risk of concussion, particularly in youth ice hockey; predicting persistent post-concussive problems; developing and testing new treatments for post-concussion syndrome; and determining readiness to return to activity.
PLAY GAME: Post-concussion syndrome Affecting Youth: GABAergic effects of Melatonin
Karen M Barlow, University of Calgary
One in seven children will have had a concussion by age ten, and 11% of those children continue to have post-concussion symptoms, include headaches, fatigue, sleep disruption, mood and concentration difficulties three months later. The neurological basis of post-concussion symptoms is not clear, although recent evidence suggests dysfunction in GABAergic neurotransmitter systems. Building on previous research, which found that 85% of children with post-concussion symptoms and sleep problems reported improvement when treated with melatonin, Dr. Barlow and her team investigated melatonin as a treatment for children with post-concussion symptoms including its pain-relieving, brain injury protective and GABAergic effects. The results of their work have the potential to provide a safe treatment for post-concussion symptoms in children and provide insight into how neuronal networks and brain connectivity change during treatment and recovery to provide even better interventions in the future.
Brain blood flow in youth concussion
Paul van Donkelaar, University of British Columbia-Okanagan
Dr. van Donkelaar and his lab study the effect of head impacts on brain blood flow in youth. They measured brain blood flow in young athletes who had a diagnosed concussion or suffered head impacts during their playing season. The team used two distinct measures – cerebral autoregulation and neurovascular – and showed that both these measures were disrupted in concussion and cases of reported head impact. As an extension of this research, they are now studying the intersection between traumatic brain injury and intimate partner violence.
SHRed Injuries: Preventing injuries and their consequences in youth sport and recreation
Carolyn Emery, University of Calgary
Dr. Emery is leading SHRed Injuries, a research program based on a comprehensive web-based injury surveillance platform developed and validated in youth sport to evaluate injury prevention strategies. Research by Dr. Emery and her team led Hockey Canada to ban body checking for players under 12 years of age, resulting in a 64% reduction in concussion risk and 50% reduction risk in injuries overall. These results prompted a body checking policy change in 13 to 17-year-old non-elite leagues with a similar impact. Dr. Emery’s team also evaluated neuromuscular training warm-up programs in sports and schools, demonstrating a reduction in the risk of injuries of more than 35%. Future research focuses on optimizing injury prevention training strategies and secondary prevention strategies for youth.
How can we best track recovery after concussion in youth?
Isabelle Gagnon, Research Institute of the McGill University Health Centre
Pediatric concussion or mild traumatic brain injury is common, but there is very little consensus among clinicians and researchers on how to diagnose and treat it. Dr. Gagnon assembled a team of clinician scientists, researchers and knowledge users from across Canada, whose innovative research programs and clinical initiatives have had a significant impact on the field of pediatric concussion. Together they selected a set of tests and questionnaires to be used with children and adolescents after a mild traumatic brain injury and determined which ones were most useful. This will now serve to help standardize research in this population. The team followed 484 children and youth aged 6 to 17 years, and an additional 100 infants and toddlers – a population which is rarely studied and for which evidence on recovery is much needed.
'NeuroCare' as an innovation in intervention: A neurophysiological approach to determine readiness for return to activity
Michelle Keightley, Holland Bloorview Kids Rehabilitation Hospital (Toronto)
To date, there are major gaps in our knowledge about how to best manage the physical and cognitive demands associated with returning adolescents to activity following mild traumatic brain injury. Returning to activities prior to the brain healing from its injury may result in delayed recovery or the increased risk for more serious brain injury. One approach to further inform when the brain and body are ready to re-engage in activity may be monitoring neurophysiological parameters. Heart rate variability is a non-invasive measure of neurophysiological function that may provide insight into when the brain and body are ready to return to activity. Dr. Keightley and her team studied the role of heart rate variability in determining neurophysiological recovery following mild traumatic brain injury in adolescents. This innovative approach will optimize clinical decision-making, educate health care professionals and improve the health outcomes for adolescents recovering from mild traumatic brain injury across Canada.
Behavioural markers from walking to detect subtle, persistent dysfunction following concussion
Bradford J Mcfadyen, Université Laval
The great majority of traumatic brain injuries are mild and often underdiagnosed. Dr. Mcfadyen and his team are seeking to better detect mild traumatic brain injuries in adolescents and young adults. To simulate the demands of daily activity, the team studied the effectiveness of a simple corridor test – a walking test – combined with multi-tasking. They used sophisticated motion analyses to observe the performance of both adolescents and young adults with and without mild traumatic brain injuries. They found the addition of multi-tasking during the test revealed subtle persistent dysfunction in participants who had suffered a mild traumatic brain injury in the preceding weeks. The results provided evidence supporting the use of a simple corridor test as a means to help clinicians make decisions about return to activity for young people with mild traumatic brain injuries.
Predicting Persistent Postconcussive Problems in Pediatrics (5P)
Roger Zemek, Children's Hospital of Eastern Ontario (Ottawa)
Dr. Zemek leads the 5P study, which is the largest prospective concussion study to date. Dr. Zemek and his team enrolled over 3000 children across nine Canadian pediatric emergency departments to derive and validate a risk score for persistent post-concussion symptoms. The 5P risk score has been implemented into a head injury screening tool by the Centres of Disease Control. The score has also been incorporated into the latest international concussion guidelines and allows clinicians to provide evidence-based anticipatory guidance to families. In addition, concussion researchers have adopted the 5P score as a tool to stratify participants by risk.
Research Profile:
Researcher guiding policy on concussions in sport
Ash Kolstad suffered a concussion playing hockey when he was 12 years old. Eight years have passed and Ash still suffers with the symptoms of persistent post-concussion syndrome, which include headaches and difficulty concentrating.
As a kinesiology student at the University of Calgary, Ash is sharing his experience and carrying out research as a member of Dr. Carolyn Emery's team at the University’s Sport Injury Prevention Research Centre. Dr. Emery and her team are helping shape sport policies that prevent concussions and improve recovery both in Canada and worldwide.
Their research prompted Hockey Canada in 2013 to ban body checking in Pee Wee ice hockey (11-12 years). In a study published in the British Journal of Sports Medicine, the team showed that this body checking policy change reduced concussion risk by 64 percent and cut the overall risk of injury in half. As a result, local and provincial hockey organizations extended the body checking ban to other age levels and divisions.
Dr. Emery played a lead role in the development of the Berlin Consensus Statement on Concussion in Sport and presented the statement to the International Olympic Committee. This international statement provides guidance to physicians and other health care professionals on the prevention, diagnosis and management of concussions in athletes. Dr. Emery continues to work with schools and community partners to promote concussion prevention strategies such as protective gear, rule changes and education programs.
Dr. Emery has received funding for her research from IHDCYH and the Institute of Neurosciences, Mental Health and Addiction, as well as the Hotchkiss Brain Institute, as part of the Traumatic Brain Injury Initiative.
Initiative introduction: Supporting the advancement and translation of scientific knowledge on cannabis in Canada
Funds committed: $0.9M
The Integrated Cannabis Research Strategy (ICRS) aims to build the evidence base on the benefits and harms of cannabis use under different contexts; establish rigorous clinical evidence for therapeutic use of cannabis; develop common data standards through coordinated investments in research; and get evidence into the hands of healthcare providers, policy makers and other knowledge users.
Despite the legalization and regulation of cannabis products for non-medical purposes in Canada, there remain many unknowns about the use of cannabis, both medical and non-medical, its health and safety effects and the behavioural, social, cultural, ethical and economic implications of legalization both nationally and across jurisdictions. To address the need for enhanced research evidence to inform policy, practice, harm reduction, medicinal use and prevention efforts, CIHR developed the ICRS in 2017. The strategy is led by the Institute of Neurosciences, Mental Health and Addiction in collaboration with IHDCYH and the Institutes of Cancer Research; Circulatory and Respiratory Health; Indigenous Peoples’ Health; and Musculoskeletal Health and Arthritis.
Understanding the health, social and economic impacts of cannabis legalization in Canada
Timeline: 2018 - 2019
The Population Health Intervention Research on Legalization of Cannabis Catalyst Grants were launched to support the prompt initiation of intervention research to assess how the legalization and regulation of non-medical cannabis in Canada is impacting population health and health equity.
Through this component of ICRS, researchers, practitioners and policymakers worked together to build an evidence base to support policy and program development in health and other sectors and to catalyse future population health intervention research involving the new cannabis legalisation in Canada. The grants supported the planning and implementation of projects that advanced our knowledge and capacity in the areas of data collection, surveillance and reporting, as well as our understanding of regulatory models and the impact of legalization on specific groups, including youth.
Targeted cannabis prevention for youth at risk for psychosis
Patricia Conrod, Centre hospitalier universitaire Sainte-Justine
One major public health concern associated with the legalisation of cannabis, is the potential to encourage more cannabis use amongst youth and consequently increase risk for substance-induced psychosis in the population. Two decades of epidemiologic research suggests that heavy and early onset cannabis use/abuse increases risk for psychosis in individuals with pre-existing vulnerability to psychosis. Dr. Conrod’s team previously demonstrated that cognitive behavioural interventions were highly effective in reducing concurrent substance use/misuse in high-risk youth. Building on this previous work, the team is developing a new targeted cannabis and psychosis intervention and prevention strategy. First, to inform the development of the new intervention, the team is collecting qualitative information from high-risk youth on the internal and external triggers for cannabis use. Next, they will evaluate the effectiveness of their intervention in reducing cannabis use and other mediators of use. Finally, they are conducting focus groups with key stakeholders to develop a feasible and sustainable implementation strategy for using the intervention within school and pediatric settings.
Influence of cannabis exposure in pregnancy on offspring perinatal and childhood health outcomes: a population-based birth cohort
Darine El-Chaar and Daniel J Corsi, Ottawa Hospital Research Institute
With the legalization and increasing social acceptability of cannabis use, more pregnant women are likely to use cannabis, but the health risks for mothers and their babies are not clear. Using medical records of delivery across all institutions in the province of Ontario to compare mothers who used cannabis and those who did not, Drs El-Chaar and Corsi and their team are studying the impacts of cannabis use on pregnancy complications and developmental impairments in children. Results from the study will inform women, medical practitioners and the government on the risks of cannabis use in pregnancy and provide evidence-based information for pregnant women and their health care providers to make safe and healthy decisions in pregnancy.
Trajectories of marijuana use across a decade: Their predictors in adolescence and impact on health, academic, social and economic outcomes in young adulthood
Bonnie J Leadbeater and Murray W Fyfe, University of Victoria
The legalization and regulation of marijuana in Canada has focused attention on youth as a sub-group of considerable concern, this is not unwarranted. Despite its previous status as an illegal drug, according to a UNICEF survey (2013), 28% of 11 to 15-year-old Canadians reported using marijuana in the last year. However, youth differ in their patterns of marijuana use - in both frequency of use and amounts used. Their patterns of use (typically called trajectories) can also change from adolescence to young adulthood. Drs Leadbeater and Fyfe and their team are examining predictors and impacts of five different patterns of marijuana use (Abstainers, Occasional Users, Increasers, Decreasers and Chronic Users) on economic, academic, social and mental health outcomes in youth. Knowledge gained from this research will inform stakeholder discussions about the selection of indicators for a Canada-wide longitudinal study that will improve our ability to monitor how youth are impacted by the legalization and regulation of marijuana.
Development of a Canadian Youth Cannabis Survey: Understanding changing aspects of cannabis use among young Canadians
Martin J. Cooke, Hanan Abramovici, Julie Laroche & Amy J. Porath, University of Waterloo
Legislation has been introduced to legalize and regulate recreational cannabis use, and an important concern is protecting young people from its potential harms. Cannabis use by Canadian youth is among the highest in the world, and although recent trends have been downwards, it is critical to monitor how these patterns change after legalization. Drs Cooke, Abramovici, Laroche and Porath and their team are conducting an analysis to identify how patterns of use change after legalization, how these trends vary by province and for population subgroups including official language minorities, youth in low income households, rural and urban youth and recent immigrants. The team is using existing data, as well as developing new surveys to collect information on youth cannabis use that has not previously been collected, such as whether cannabis was obtained from illegal sources, forms of cannabis used and the price paid, among other questions. The team’s analyses, surveys and focus groups will inform future survey development and data collection and contribute to our understanding of the impact of legalization on cannabis use by youth.
Addressing urgent cannabis research priorities in Canada
Timeline: 2019 - 2020
The Cannabis Research in Urgent Priority Areas Catalyst Grants funding opportunity supports the generation of new knowledge in target research areas.
Research funded through this set of Catalyst Grants will strengthen the evidence base, build capacity and expand cannabis research in key areas such as neurodevelopment, mental health, cannabis and pain management, social determinants of health and key populations, potency and product safety, cannabis and other drug/substance use, and prevention, harm reduction and treatment of problematic cannabis use.
Assessing the impacts of the Cannabis Act on patterns of motor vehicle collision injuries among youth and young adults in emergency departments across Canada
Russell C Callaghan, University of Northern British Columbia
The Canadian Pediatric Society and the Canadian Association of Chiefs of Police have expressed concern about how cannabis legalization might exacerbate patterns of motor vehicle collisions among young people. Cannabis-impaired driving is now more prevalent among adolescents than alcohol-impaired driving, and individuals aged 15 to 24 years have the highest annual numbers of national emergency department admissions for motor vehicle collision injuries. The Cannabis Act imposes a federal minimum-age restriction for the sale of cannabis products to individuals at least 18 years of age (minimum legal cannabis age), with provinces having the mandate to set increased age limits. Using emergency room data from across Canada, Dr. Callaghan and his team are assessing the impacts of cannabis legalization on patterns of motor vehicle collision injuries among youth who are younger than the minimum legal cannabis age and young adults who are older than the minimum legal cannabis age. The team expects that the implementation of the Cannabis Act will be associated with significant increases in patterns of injury due to motor vehicle collisions among young adults just older than the provincial/territorial minimum legal cannabis age.
Shared and specific risk factors for early onset cannabis and other substance use and later substance use disorders: Can we predict who will initiate cannabis use early and who will develop future substance use problems?
Natalie Castellanos Ryan, Centre hospitalier universitaire Sainte-Justine
One in three Canadian youth in the 16 to 25 age group are active cannabis users, with statistics showing that trends in cannabis use are rising. Some studies have shown that cannabis use during adolescence is associated with higher risk for adult cannabis and other substance use disorders; however, it is still unclear whether starting cannabis use earlier in adolescence puts youth at higher risk of developing later substance use problems when accounting for early risk factors, environmental factors and different patterns of substance use. Building on an ongoing longitudinal study, Dr. Castellanos Ryan and her team are collecting data on cannabis and substance use, youth mental health and environment to determine whether the association between cannabis use initiation and later substance use problems remains when considering these important factors. This study has the potential to help guide policy and prevention for those more likely to develop substance use problems by early adulthood.
Parental cannabis use in the perinatal period and child outcomes: Capturing changes with legalization in the Ontario Birth Study
Julia A Knight, Sinai Health System
Cannabis use is increasing among women and men during the ages when they are most likely to have children. There is some evidence that cannabis use during pregnancy can affect child development, but this evidence is inconsistent. Using data collected through the Ontario Birth Study – an ongoing study that recruits women during pregnancy and follows them until after birth – Dr. Knight and her team are studying the effects of cannabis use during pregnancy on birth weight, brain development and child development at 24 months and 4 years. They are also looking at how cannabis use during pregnancy changes with legalization and what factors are associated with its use. This information will be important in developing a larger study to look at how cannabis use might affect children over the long term.
Secondary prevention of cannabis-related harms among youth and young adults: A pilot RCT
Igor Yakovenko, Dalhousie University
Researchers recognize that only a small portion of individuals with cannabis-use problems ever seek treatment. Therefore, effective interventions are urgently needed to meet the needs of people who already use cannabis, but who are not currently receiving specialty treatment for cannabis addiction. The impact of providing an easily accessible intervention platform for cannabis problems has not been evaluated. To address this issue, the Canadian Research Initiative on Substance Misuse (CRISM) is developing an online intervention platform (Screening, Self-Management and Referral to Treatment; SSMRT) that is accessible to the general public and intended to provide online access to screening and intervention resources. Using an online survey and focus groups, Dr. Yakovenko and his team will evaluate whether using the SSMRT program reduces problems associated with using cannabis, ways in which to improve SSMRT and how to make it more accessible. The information gathered will be used to support university programming and service development to help students with cannabis use concerns.
Enabling Tactics
Tactic: Strengthen research capacity in family, child and youth health
Ensuring that the family, child and youth health research community is strong and vibrant was a critical element in addressing IHDCYH’s strategic priorities.
Between 2012 and 2019, IHDCYH followed a comprehensive approach to training and capacity building that recognized multiple needs along the research career pipeline including provision of support for trainees, early- and mid-career researchers; identification of gaps in under-represented fields; and solutions to address barriers to entry into research/remaining in research. As well as the targeted initiatives described in this report, IHDCYH partnered on a number of other funding opportunities and provided educational activities and resources to trainees and early-career investigators.
IHDCYH is also supporting the Network Environments for Indigenous Health Research (NEIHR) Program, a $100.8M investment over 16 years that has been developed to address needs in capacity development, research and knowledge translation in Indigenous research. Led by the Institute of Indigenous Peoples’ Health (IIPH) and co-led by the Institute of Circulatory Health (ICRH), the program supports a national network of centres that provide research environments for Indigenous health research driven by, and grounded in, Indigenous communities in Canada. The centres are taking a comprehensive approach to capacity building in Indigenous health research by concentrating on Indigenous community and structural factors and by focusing on individual agency along the entire career continuum.
As well as building capacity along the career continuum, IHDCYH sought be expand capacity into specific research areas, notable artificial intelligence (AI). Traditionally, expertise in AI has been held within the IT and engineering disciplines. Through the Collaborative Health Research Projects (CHRP): Special Call – Artificial Intelligence, Health and Society funding opportunity, IHDCYH built capacity by encouraging researchers in our community to collaborate with researchers with expertise in AI to tackle problems relevant to our mandate. The successful applications included two virtual or robotic support systems for children with disabilities or chronic conditions and two methods for using AI for clinical prediction, assessment and intervention.
IHDCYH’s capacity building strategy: supporting researchers at critical points along the research career pipeline
Supporting early career investigators
Funds committed: $22.6M
Timeline: 2012 onwards
To provide promising early career investigators in family, child and youth health with a step-up at the beginning of their independent research careers, IHDCYH supports two funding programs that complement each other.
These two programs are the SickKids Foundation-IHDCYH New Investigator Research Grants program, which is administered by the SickKids Foundation in partnership with IHDCYH, and the CIHR Early Career Investigators in Maternal, Reproductive, Child and Youth Health, which is a partnership between IHDCYH and other CIHR institutes with an additional funding match provided by partners obtained by the applicants, most often their host institution. Both programs include annual funding opportunities that support research related to any area of IHDCYH’s mandate.
The SickKids Foundation-IHDCYH New Investigator Research Grants program has been funding early career investigators since 2001. During this time, 160 grants totaling $30M have been awarded, of which 37 grants totaling $9.1M were awarded during Dr. Lee’s tenure as IHDCYH SD. The CIHR Early Career Investigators in Maternal, Reproductive, Child and Youth Health program has been running since 2017, and has so far funded 59 early career investigators in 19 institutions across Canada who are working in a wide range of research areas in family, child and youth health. While it is too early to evaluate the contribution of the Early Career Investigators in Maternal, Reproductive, Child and Youth Health program to increased research capacity, the longer-running SickKids Foundation-IHDCYH New Investigator Research Grants has been very successful and many of the grant recipients have established highly productive research careers and become leaders in their fields.
Recipients of a SickKids Foundation New Investigator Research Grant include
- Dr. Simone N. Vigod (2014), whose research focuses on women with mental health issues and their journeys prior to, during, and after pregnancy, and who now leads the Reproductive Life Stages Program at the Women’s College Hospital, Toronto;
- Dr. Pia Wintermark (2013), who investigates brain damage in newborns and is Director of the NeoBrainLab at Montreal Children’s Hospital;
- Dr. Kym Boycott (2010) at CHEO, who identified a novel gene for Joubert syndrome and went on to secure $20M+ in funding to support a national network to use next generation sequencing to discover genes for rare diseases;
- Dr. Jocelyn Gravel (2009), who studies pediatric head trauma and emergency pain management, and is now the Director of Research in the Emergency Department of CHU Sainte-Justine;
- Dr. Steven Miller (2007), who researches neonatal brain injury and development and is now Head of Neurology and of the Centre for Brain & Mental Health at SickKids; and
- Dr. Stuart Turvey (2006), Director of Clinical Research at BC Children’s Hospital, whose research focuses on the role of the immune system in childhood disorders.
Tactic: Translate knowledge for better application of evidence
As well as investing in family, child, and youth health research, IHDCYH has an important role in stimulating and supporting translation of the knowledge gained from that research.
In addition to our grant funding opportunities, we actively seek to build a sense of community, inform our different stakeholder groups (researchers, funders, community members, policy makers and others) and bring them together, as well as facilitate knowledge translation through a variety of activities. These approaches have included a Facebook Live event celebrating World Breastfeeding Week; a Policy Research Dialogue in Injury Prevention; and Café Scientifiques discussing research on sleep disturbance and brain development, bullying, child and youth mental health services, and hidden chemicals in household products, among others. We also release a biweekly ebulletin, are active on social media, and run a video competition called IHDCYH Talks.
Online
- Ebulletin: 804 subscribers, 41.2% open rate
- Twitter: 2,015 followers, 138K views / month
- Website: 41K views / year
- YouTube: 407K totals views, 845 subscribers
IHDCYH Talks: Translating knowledge via video
Our IHDCYH Talks video competition has been running for 6 years, and gaining momentum and international exposure. Each year, short videos with easy-to-understand, evidence-based messages relevant to IHDCYH’s mandate are submitted and peer reviewed. Public viewer voting also helps to decide which video will win the top prize. The competition directly enhances the profile and reach of the entrants, not only through the widely publicised voting component, but also through subsequent promotion and dissemination activities that highlight the winners through various social media channels.
Winning videos include:
- It doesn't have to hurt: The power of a parent's touch in reducing baby's pain during medical procedures, Marsha Campbell-Yeo, IWK Health Centre (2014)
- The CHILD Study whiteboard video, Judah Denburg, McMaster University (2015)
- 3 Ways to Instantly Relieve your Baby's Pain, Christine Chambers, IWK Health Centre (2016)
- Pathways in ASD Study - A family's story, Peter Szatmari, Centre for Addiction and Mental Health (2017)
- Smart discharges to improve outcomes among pediatric sepsis survivors in low & middle income countries, Matthew Wiens, University of British Columbia (2018)
- HIV transmission through breastfeeding, Lena Serghides, University Health Network (2019)
IHDCYH Talks impacts:
| Total views | 407K |
|---|---|
| Mean view time | 1 min 37 seconds |
| Viewer location | |
| Canada | 33% |
| United States | 29% |
| United Kingdom | 6% |
| Other countries | 32% |
| Total views during voting period | |
| 2014 | 21,175 |
| 2015 | 20,989 |
| 2016 | 12,050 |
| 2017 | 27,093 |
| 2018 | 38,481 |
| 2019 | 52,033 |
Online comments:
“As a former oncodad and tireless childhood cancer advocate I tip my hat and salute all involved in this project and will promote it globally”
“Excellent resource for parents and health professionals.”
“Great info shared in a way that is easily understood without being condescending. Repetition of key points was supportive.”
“This is a fantastic video and such an amazing resource and I hope to use it with our undergraduate nursing students for pre-learning for simulation. It is perfect as it is a great overview of the care and management of a child with bronchiolitis. Thank you very much for this!”
Tactic: Develop and sustain effective partnerships and collaborations
Central to IHDCYH’s impact on family, child and youth health research is our role as convener and catalyst for our community.
By collaborating directly with funding partners and other organizations both national and international—including the SickKids Foundation, World Health Organization (WHO), the National Natural Science Foundation of China, the Indian Department of Biotechnology, and the South African Medical Research Council—IHDCYH was able to build strong and lasting partnerships that leverage significant funds for investment in research, such as our ongoing partnership on the SickKids Foundation-IHDCYH New Investigator Research Grants and the $42.68M invested in HeLTI.
We also actively sought to promote linkages between researchers, funders, community members, policy makers and other stakeholders. Between 2012 and 2019 we funded 47 planning grants to bring researchers together to develop new research ideas. On an ongoing basis, we also engage with professional organizations and stakeholder groups at conferences, such as the Canadian Association of Paediatric Health Centres, Canadian Paediatric Society, Canadian National Perinatal Research Meeting, and Society of Obstetricians and Gynaecologists of Canada, several of whom also partner on our grants to support networking and knowledge translation.
Tactic: Embrace global health
Over 2012 to 2019, IHDCYH has taken a strategic approach to investment that considers the opportunities offered by global health research.
Lower-income countries face unique challenges compared with those faced by high- and middle-income nations. Research also indicates that low-income countries can generate effective solutions for today’s global health challenges, and can help inform health systems in developed countries. The greatest example of this is HeLTI, which partners Canadian researchers with researchers from three other countries to identify interventions against non-communicable diseases that will have applications worldwide. IHDCYH also supported the Innovating for Maternal and Child Health in Africa (IMCHA) initiative in partnership with Global Affairs Canada and the International Development Research Centre (IDRC).Through the initiative, 19 implementation research teams led by African and Canadian researchers and health policymakers are developing practical solutions to improve support and health care for women and children in their communities.
Tactic: Facilitate data access and sharing
Within Canada a wealth of research data is being generated through various means including a large number of cohorts and databases.
However, access to and sharing of data is an ongoing challenge for researchers due to the siloed nature of grants and projects, as well as federal and provincial policies and legislation. Over the last eight years, IHDCYH has focused on facilitating data cataloguing, sharing, access and dissemination through several of our research investments, including HeLTI, the Canadian Urban Environmental Health Research Consortium (CANUE), the Canadian Microbiome Initiative 2: Research Core and grants to support access to and analysis of existing data.
In HeLTI, data harmonization, access and linked analysis are core principles of the four HeLTI Linked International Interventional Cohorts, while the Canadian DOHaD Cohort Registry (known as ReaCH) is providing a platform that can facilitate larger and better-powered studies among relevant cohorts. CANUE is working to link environmental data about air quality, green spaces, walkability, noise and other aspects of the urban/suburban environment with existing human health data, which includes a number of pregnancy and child cohorts. This data is then being made available to any interested researchers. The Canadian Microbiome Initiative 2: Research Core (known as IMPACTT) is acting as a central platform for coordination and access to genetic and metabolic data on a large repository of microbes.
Thanks, IHDCYH team members past and present
IHDCYH staff
Scientific Director
Shoo K. Lee
Assistant Directors
Sarah De La Rue
Elisabeth Fowler
Sukhy Mahl
Cecilia van Egmond
Associates
Ruth Warre
Marlene Greenberg
Emily Torr
Project Officers
Shohi Prajapati
Rhiannon Renaud
Lynne Renaud
Finance and Administrative Officer
Cynthia Yeh
Administrative Assistants
Nerizza Matignas
Carlena St Brice
Institute Advisory Board
- Anne Monique Nuyt
- Fabiana Bacchini
- Peter Gill
- Sara Kirk
- Peter Leung
- Stephen Matthews
- Sarah McDonald
- Steven Miller
- Prakeshkumar Shah
- Cecilia Van Egmond
- Robert Viger
- Roberta Woodgate
- Frank Gavin
- Rima Azar
- Erik Skarsgard
- Leanne Boyd
- Alan Bocking
- Stephen J Lye
- Vassilios Papadopolous
- Astrid Guttman
- Nora (Noni) MacDonald
- Elaine Orrbine
- Anne Snowdon
- Bernard Robaire
- Reg Sauve
- Bonnie Leadbeater
- Charlotte Waddell
- John LeBlanc
- Ellen Hodnett
- Karen Lloyd
- Peter Mitchell
- Jean-Marie Moutquin
- Gina Muckle
CIHR Integrated Institute Team
- Courtney Acott
- Michael Smolinski
- Andre Fortin
- Michael Urgolo
- Hana Kokanovic
- Andrew McColgan
- Abby Forson
- Kim Beaumont-Vaillancourt
- Shawna Healy
- Anita Ploj
- Allison Forsythe
- Sara Harbord
- Mary Fraser Valiquette
- Lynn Knight
Partners
A heartfelt thank you to each and every partner that has helped IHDCYH improve the health of Canadian children, youth and their families! The work outlined in this report could not have been possible without your support.
Appendix 1: Total funding committed from 2012 to 2019Footnote 1
| CIHRFootnote 2 | External partners | Total | |
|---|---|---|---|
| Healthy Developmental Trajectories | |||
| Developmental Origins of Health and Disease through the Lifespan | $35.0M | $7.9M | $42.9M |
| Preterm Birth | $6.6M | $4.3M | $10.8M |
| Healthy Reproduction, Pregnancy, Childhood and Youth | |||
| Environmental Health | $37.1M | $1.5M | $38.6M |
| Healthy Pregnancy | $3.7M | $3.7M | $7.5M |
| Healthy Public Policy and Systems Integration | |||
| Integrated Child and Youth Research and Health Services | $26.5M | $7.8M | $34.3M |
| Mental Health | $16.8M | $9.0M | $25.8M |
| Enabling Tactics | |||
| Capacity Building | $21.2M | $20.4M | $41.6M |
| Knowledge Translation | $0.7M | $0 | $0.7M |
| Data Sharing | $2.8M | $0 | $2.8M |
| Total | $150.4M | $54.6M | $205.M |
- Date modified: